INTRODUCTION
Primary tumors in the airway are very rare, with primary tracheal tumors occurring at a rate of 0.1 per 100000 people each year1. According to the World Health Organization (WHO), spindle cell carcinoma accounts for less than 1% of cases2. This type of tumor consists of spindle-shaped epithelial cells arranged in an irregular pattern, often with darkened nuclei and different nucleolus sizes1.
Therapeutic bronchoscopy is often used as a palliative option for tumors that cannot be removed but cause central airway obstruction (palliative unresectable tumors)3,4. However, bronchoscopy ablation alone may not work well for spindle cell sarcoma due to its tissue structure. In such cases, airway stents can be an alternative to maintain an open airway. Definitive therapy, such as radiotherapy or chemotherapy, can then be administered to improve the outcome.
CASE PRESENTATION
A 49-year-old Javanese woman presented to the emergency department with a chief complaint of shortness of breath for one year, which had worsened over the prior week. She denied having difficulty swallowing or experiencing nausea or vomiting. The patient had had a history of pulmonary tuberculosis one year prior but no history of malignancy. Upon examination, she was conscious but in respiratory distress. Auscultation revealed stridor and bilateral vesicular breath sounds without crackles or wheezing.
Radiological examination showed evidence of previous pulmonary tuberculosis with a superior central mass on the right side and mucous impaction. A solid mass was observed in the tracheal lumen at the thoracal 3–4 level, which was compressing the esophagus. The patient was a passive smoker and had a history of diabetes mellitus, for which she regularly used insulin. Laboratory findings, including hemoglobin, leukocyte count, platelet count, random blood glucose, liver function, and kidney function, were within normal limits. Tumor markers were also within normal limits: carcinoembryonic antigen (CEA) 2.6 ng/mL, beta-human chorionic gonadotropin (B-HCG) <2.30 mIU/mL, alpha-fetoprotein (AFP) 3.78 ng/mL, and lactate dehydrogenase (LDH) 187 U/L.
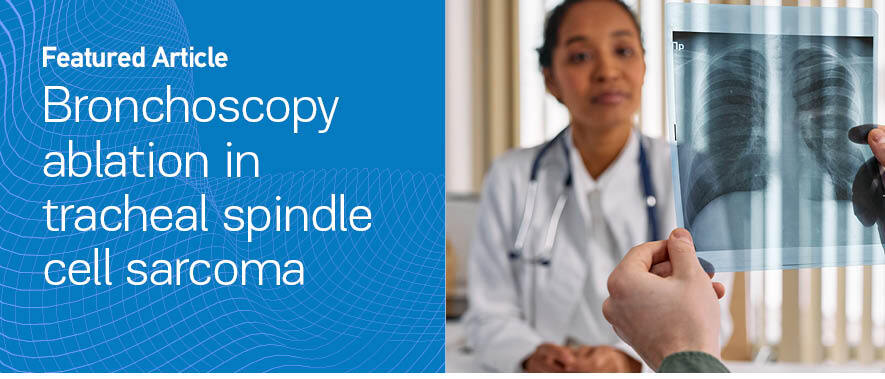
After obtaining the patient’s consent, a therapeutic bronchoscopy was performed. The bronchoscopy examination revealed an infiltrative tracheal mass almost completely obstructing the lumen, located 1 cm from the carina and extending 3.5 cm from the posterior tracheal wall (Figure 1A). Ablation with a neodymium yttrium aluminum garnet (Nd-YAG) laser was performed, followed by rigid bronchoscopy for mass removal. However, only a small portion of the mass was successfully evacuated. As the tracheal lumen remained >50% obstructed post-procedure, a Y Dumon silicone stent was placed (Figures 1B and 1C). After therapeutic bronchoscopy, the tracheal lumen was patent, ventilation was adequate and the patient remained hemodynamically stable without bleeding, pneumothorax, or other complications. The patient no longer experienced shortness of breath.
Figure 1
Bronchoscopy imaging before and after stent placement in tracheal spindle cell sarcoma: A) Bronchoscopy revealed a large, hypervascular tumor obstructing nearly the entire tracheal lumen; B) Bronchoscopy after mass removal using a rigid scope and laser application showed a residual mass obstructing the trachea; C) A silicone stent was placed to maintain airway patency; D) Bronchoscopy after stent removal showed good airway patency
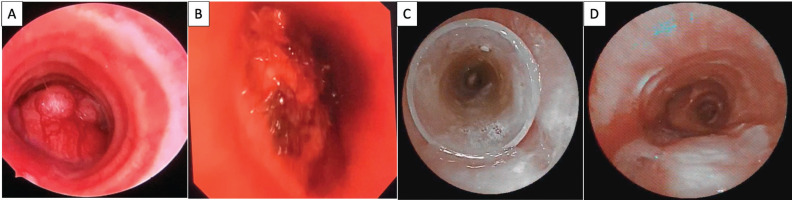
Histopathological examination confirmed a low-grade spindle cell sarcoma, with tumor morphology suggesting a low-grade malignancy of neural differentiation. Immunohistochemical staining showed positive S100 and Ki-67 expression in a small number of cells (Figure 2). There were no epidermal growth factor receptor (EGFR) exon 19 deletions or L858R mutations, and no anaplastic lymphoma kinase (ALK) mutation. Due to health insurance limitations, this case was not tested for MET exon 14 mutations, programmed death ligand 1 (PD-L1), or other molecular examinations beyond EGFR and ALK mutation testing.
Figure 2
Histologic and immunohistochemical features of spindle cell sarcoma: A) Hematoxylin-eosin staining showing cellular haphazardly arranged spindle cell proliferation with prominent stromal hyaline collagen bands (×400); B) Immunohistochemistry showing positive S100 (×400); C) Immunohistochemistry showing positive vimentin (×400)
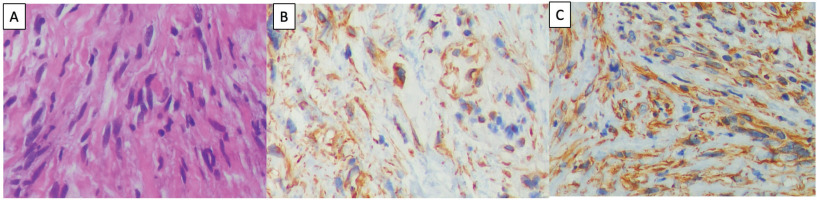
The patient subsequently underwent external radiation therapy using conformal radiotherapy, which delivered a total dose of 70 cGy fractionated into 30 sessions. Following radiation therapy, chemotherapy was administered with a regimen of carboplatin at 175 mg/m² and paclitaxel targeting a cumulative exposure (AUC) of 5 mg/mL/min over six cycles in three-week intervals. Post radio-chemotherapy, the patient reported productive coughing. A repeat chest computed tomography (CT) scan revealed a widened tracheal lumen. The bronchoscopy evaluation showed mucoid hypersecretion. Bronchial lavage culture identified Pseudomonas aeruginosa. Stent removal was performed (Figure 1D). Chest CT scans conducted one year and two years after stent removal revealed atelectasis, with a tumor size comparable to the previous evaluation and no intraluminal mass (Figure 3).
Figure 3
Chest CT images and timeline of treatment: A) Coronal view of the mediastinal window showing a mass in the middle trachea; B) After laser and rigid bronchoscopy mass removal, a coronal view of the mediastinal window shows an open airway with stent (red box); C) After chemoradiation and stent removal, a coronal view of the mediastinal window shows airway patency; D) Two years after chemoradiation and stent removal, a coronal view of the mediastinal window showed airway patency; E) Timeline of treatment
DISCUSSION
Spindle cell sarcoma is a rare malignancy that originates from poorly differentiated non-small cell carcinoma and is commonly referred to as sarcomatoid carcinoma5. Pathologically, spindle cell carcinoma is predominantly composed of spindle-shaped epithelial cells that typically lack differentiated carcinoma elements. Sarcomatous lesions are typically large, which leads to a narrowing of the tracheal diameter by more than 50%. In this case, the tumor exhibited low-grade spindle cell morphology, with positive S100 protein staining. The possibility of a malignant tumor with neural differentiation with low-grade histology cannot be ruled out. Additionally, the possibility of higher grade spindle cell tumor involvement in other areas that are not biopsied remains.
Due to its rarity, there are currently no specific guidelines for spindle cell carcinoma, particularly in the central airway. Multidisciplinary tumor board recommendation is essential, especially in cases of complicated central airway obstruction. Appropriate management can be lifesaving.
The type of central airway obstruction in this case was a mixed type that involved both intraluminal mass and external compression. Therefore, the initial management steps were ablation and mass evacuation via bronchoscopy. The choice of ablation modality primarily depends on the availability of equipment and the operator’s expertise. We decided to use a laser. Laser ablation can penetrate deep into tissue but carries a risk of tissue edema4. The combination of laser ablation and mechanical removal can improve recanalization effectiveness and clinical outcomes for patients6,7. In this case, the tumor in the endotracheal airway was sufficiently large and was not prone to bleeding. However, after ablation and mechanical removal, recanalization was not fully achieved. Insertion of an airway stent was performed to maintain airway patency until the patient could undergo definitive therapy. Stent placement was recommended to extend beyond the stenotic segment; therefore, a Y-stent was chosen to cover the carina. A silicone stent was selected because a previous study had reported a higher overall complication risk with metallic stents, despite both types having similar efficacy and safety profiles8. Stent insertion is generally only recommended for patients who will not undergo surgical resection. Surgical resection is the definitive treatment for primary tracheal tumors. Tumor resectability depends on locoregional characteristics and is associated with better survival rates compared to palliative therapy, particularly if complete resection is achieved5.
Several retrospective studies indicated that resection combined with adjuvant radiotherapy yields better clinical outcomes than either resection alone or radiotherapy alone. Several case studies have utilized chemoradiotherapy with cisplatin-based, docetaxel-based, and carboplatin-based regimens as surgical adjuvants in cases of sarcomatoid carcinoma1,9. However, the limited number of spindle cell tumor cases makes it challenging to conduct randomized controlled trials (RCTs) to determine the optimal treatment. Recently, there was a recommendation to perform MET exon 14 skipping mutation as routine clinical testing in pulmonary sarcomatoid carcinoma patients who may benefit from MET inhibitors10. Immune checkpoint inhibitors either as monotherapy or in combination with chemotherapy also have shown benefits in first-line therapy for advanced disease11. Due to limitations in health coverage, this patient did not undergo MET exon 14 skipping mutation and was not given durvalumab as a potential immunotherapy option.
CONCLUSION
This article presented a case of a middle-aged, non-smoking woman with spindle cell sarcoma of the trachea and central airway obstruction. The patient underwent treatment with laser therapy and rigid bronchoscopy for mass removal, followed by the placement of a silicone airway stent and subsequent radiation and chemotherapy. After radiation and chemotherapy, the airway stent was removed, and the airway remained open. A two-year follow-up confirmed that the airway remained patent, with evaluations indicating stable disease. However, this case report has limitations, including the lack of comprehensive molecular testing and its single-case nature, which limits generalizability. Further studies and detailed molecular profiling are needed to confirm long-term outcomes. Tumor ablation using a laser followed by airway stenting and subsequent radiation chemotherapy may serve as an alternative treatment for unresectable tracheal spindle cell sarcoma with central airway obstruction. Re-biopsy and further molecular testing may be necessary in this case.