INTRODUCTION
Heterotopic ossification (HO) is abnormal bone formation outside the skeletal system, often in soft tissues surrounding joints. HO results from genetic disorders, like progressive osseous heteroplasia and fibrodysplasia ossificans progressiva (FOP), or acquired conditions including bone fracture, amputation, hip arthroplasty, burn, spinal cord injury (SCI) and traumatic brain injury (TBI)1.
Recent publications suggest HO as a non-traumatic sequela of severe COVID-19. The pathogenesis of HO and its association with COVID-19 is unclear. Prolonged immobilization and systemic inflammation may play a role. Cytokine storm associated with COVID-19 upregulates factors linked to HO formation1.
We present a patient with increased body mass index (BMI) and severe COVID-19, requiring ICU admission and mechanical ventilation (MV), complicated by widespread HO. A CARE Checklist is provided in the Supplementary file.
CASE PRESENTATION
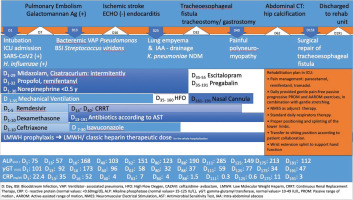
A 47-year-old hypertensive male with a BMI of 40 (kg/ m2) was admitted intubated to our ICU in October 2023, due to respiratory failure from SARS-CoV-2 infection. He was sedated, mechanically ventilated and supported with low doses vasopressors, receiving remdesivir and dexamethasone per guidelines. Complications included thromboembolic events (pulmonary embolism, stroke) and sepsis (bloodstream infections, ventilator-associated pneumonia, lung empyema, subdiaphragmatic and retroperitoneal abscesses) leading to multiple organ failure with acute kidney injury requiring renal replacement (Figure 1). A tracheoesophageal fistula developed and tracheostomy and gastrostomy were performed. Following sedation cessation, the patient regained full alertness but developed painful polyneuromyopathy. An abdominal CT scan for sepsis revealed calcifications near the hip joints and muscles (Figure 2). Painful limited passive joint movement in hips and other joints, along with CT findings, prompted further evaluation. Clinical evaluation revealed severe weakness, pain and passive movement limitations particularly in the right elbow, and bilaterally in hips and knees, but no signs of joint inflammation. The range of motion (ROM) was detected as normal on the other joints. Differential diagnosis like septic arthritis, hematoma, fracture, dystrophic calcification (DC), and FOP were ruled out. The patient did not fulfill septic arthritis criteria, since there were no other local or systemic symptoms of joint inflammation, nor did the imaging studies reveal any fluid accumulation. Hematoma or fracture were ruled out by CT studies. The intense pain and the ossification on CT were inconsistent with DC, which typically lacks pain while calcium deposits are amorphous. FOP was excluded due to the absence of hallmark big toe malformation at birth.
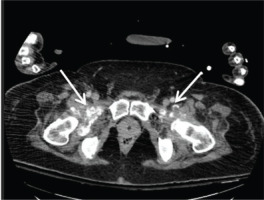
Clinical findings and abdominal CT revealed calcifications in muscles adjacent to hips (Figure 2). Radiographs of the knees and right elbow (Figures 3 and 4) demonstrated widespread HO. A Three-phase bone scan (Figure 5) demonstrated additional HO in the right humerus head and the soft tissue between the inferior angle of the left scapula and thorax. Laboratory results showed parallel increases in alkaline phosphatase (ALP) and γGT until day 65, when γGT normalized while ALP remained elevated.
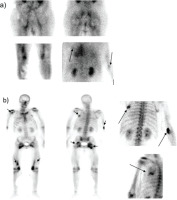
Figure 5
Three-phase bone scintigraphy indicating active heterotopic ossification: a) Blood-pool images demonstrating increased uptake of the radiopharmaceutical in the upper thoracic wall posteriorly on the left, in the right elbow area, the hip-joints’ area, the thighs and knees; b) Οsseous metabolism phase (whole body and static images) demonstrates increased uptake of the radiopharmaceutical in the left upper thoracic area posteriorly, the right elbow, the hip-joints’ area, the thighs and the knees, respectively, to the blood-pool phase, and in the right humerus head area (indicatively see arrows)
Following the HO diagnosis, a comprehensive clinical assessment identified rehabilitation needs. A tailored rehabilitation program was implemented by a multidisciplinary team, to address both acute and long-term consequences of HO along with Critical Illness Polyneuropathy and Myopathy (CIPM). Pain management included paracetamol and opioids, starting with remifentanil intravenously and transitioning to oral tramadol. Non-steroidal anti-inflammatory drugs (NSAID) and bisphosphonates were excluded due to limited effectiveness in preventing bone formation. Radiotherapy was not considered due to multi-site HO.
Early active mobilization was hindered by HO-related pain and CPIM-induced weakness. Neuromuscular electrical stimulation (NMES) was applied to prevent muscle atrophy. Gentle, pain-free passive and active-assisted ROM exercises and gentle joint stretching were provided daily for ROM maintenance. Standard respiratory therapy and pressure ulcer prevention through proper positioning and splinting were also implemented. The patient was mobilized to a sitting position as tolerated and a wrist extension splint supported hand function before ICU discharge.
Following sedation discontinuation, psychological support was provided with escitalopram and pregabalin prescribed. Family engagement was encouraged through extended visitation. Rehabilitation goals were regularly updated. Patient and family were informed about HO progression, potential complications, and the rehabilitation pathway, including possible of surgery post-ICU.
Following tracheoesophageal fistula repair and 191 days in the ICU, the patient was transferred in the Physical Medicine and Rehabilitation (PMR) Department of another hospital for full recovery, since acute and subacute COVID-19 complications had subsided but severe impairments remained.
DISCUSSION
HO is well-documented in traumatic SCI, TBI and hip surgeries, often called neurogenic HO, and has been recently reported as an atraumatic complication of COVID-19. A review2 of 15 reports on 20 COVID-19 patients with HO demonstrated that our patient shared key characteristics including hypertension, prolonged ICU stay with MV and timing of HO diagnosis around 2.8 months. However, he was younger, had a high BMI and his hospitalization was complicated by ischemic stroke, an additional HO risk factor. His HO was more extensive, affecting six sites, similar to the case from Vardar et al.3. Our patient is still undergoing rehabilitation, showing partial recovery, able to assume an upright position and walk with a walking aid.
HO is common in severe illness with prolonged systemic inflammation, typically resulting from high-energy trauma or neurological injury. Neuromuscular blockade for respiratory failure has been associated with HO, likely due to muscle denervation4. HO pathophysiology involves changes in local circulation, metabolism, and biochemistry from prolonged muscle denervation. It is important to consider HO in all critically ill patients requiring MV and muscle relaxants. Obesity, characterized by chronic low-grade inflammation, increases the release of tumor necrosis factor-alpha (TNF-α), transforming growth factor-β and interleukin (IL)-65. These proinflammatory cytokines stimulate osteogenesis and abnormal bone formation. The latter are the final endpoint of the altered metabolic pathways promoted by increased leptin levels, resistance to insulin and hyperinsulinemia that characterize obesity. We assume that obesity-induced chronic low-grade inflammation combined with other risk factors mentioned, increased our patient’s risk of HO. The link between obesity and HO was first described by Mourad et al.6 who found morbidly obese patients experienced a higher percentage of symptomatic HO after surgical repair of a displaced acetabular fracture, despite prophylactic radiation therapy (RT) or indomethacin. In COVID-19, neuromuscular blockers and prolonged immobility may confer to HO, with cases primarily involving mechanically ventilated individuals2,7,8.
Other suggested COVID-19-related contributors to HO development include systemic inflammation, regional tissue hypoxia, and deranged calcium metabolism. Acute COVID-19 studies show significant immune responses that contribute to inflammation and critical illness, with elevated inflammatory markers [C-reactive protein (CRP), IL-6 and lactate dehydrogenase (LDH)]. This inflammatory response may trigger HO. BMP1 receptor inhibitors decrease IL-6 and osteogenesis, suggesting a link between IL-6 and HO8,9.
Early recognition of HO is crucial for better patient outcomes. HO typically presents as swollen, painful joints with limited ROM, typically in the knees, hips or shoulders of COVID-19 ICU patients10. In intubated and sedated patients, diagnosis is challenging and symptoms are often attributed to overall joint capsules’ stiffness or muscle shortening from prolonged immobility. HO management in ventilated COVID-19 patients is essential for improved patient outcomes.
Early-stage diagnosis is aided by bone scintigraphy and ultrasonography, while plain radiography- though commonly used, often detects HO after 1–2 months11. CT scans may uncover HO incidentally, as demonstrated in our case.
Preventing and managing HO after trauma or cerebrovascular insult includes a combination of methods such as physiotherapy, medical management, radiotherapy and surgical removal. Therefore, no medication reverses already formed HO7. Once clinically significant HO has developed, treatment options are essentially limited to NSAIDs for pain relief, physical therapy (PT) and lastly surgical removal in cases of non-responders with functional disability11.
Given the limited literature on COVID-19 patients with HO, healthcare providers may consider NSAIDs and/ or bisphosphonates to prevent HO in high-risk patients, namely those on MV. In the discussed case, we avoided indomethacin due to advanced ossifications and potential medication interactions.
PT remains the most commonly used treatment in HO following COVID-19 but remains controversial2. In animal models, forcing muscles to ROM exercises was linked to ectopic bone formation, making PT less favorable. However, passive stretching is now believed to help preserve ROM in HO patients12. Timing and type of PT exercises for HO remain under research.
Strengths and limitations
Our case report presents a novel hypothesis linking severe COVID-19 and obesity to the development of HO. Therefore, it contributes to the limited literature on COVID-19-associated HO, encourages further investigation into this relationship, and emphasizes the importance of early HO recognition and management in critically ill patients. However, it has several limitations: the presence of ischemic stroke as a confounding factor for HO, the lack of follow-up data limits long-term outcome evaluation, and the absence of a control group restricts the generalizability of the findings.
CONCLUSION
COVID-19 associated HO has been rarely documented in medical literature, with the majority of cases reported in elderly patients with multiple medical conditions. Additionally, an association between morbid obesity and the risk of HO formation as an atraumatic complication of COVID-19 infections has never been reported. To obtain a more comprehensive understanding of the relationship between severe SARS-CoV-2 infection and HO, further research is necessary. Long-term studies that track COVID-19 patients over an extended period, assessing their bone health and identifying cases of HO, would significantly contribute to our understanding of this potential link.