INTRODUCTION
Thymoma is an uncommon malignancy, extremely unusual in children and young adults, which reaches a peak in 70-year-old individuals1. Thymomas are tumors derived from thymic epithelial cells and have an overall incidence of 0.15 per 100000 individuals per year2. Non-small cell lung cancer (NSCLC) is the commonest type of lung cancer and the main cause of morbidity and mortality in Greece. The prognosis of NSCLC depends on early detection and supply of optimal therapy. The patients’ quality of life and improvements of life expectancy are based also on avoidance of unnecessary invasive and non-invasive procedures3. We describe, for the first time, a rare case of concomitant thymoma and adenocarcinoma unilaterally in the same lung, which was treated successfully with radical surgical resections of both lesions concurrently.
CASE PRESENTATION
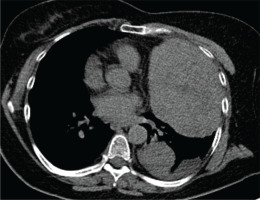
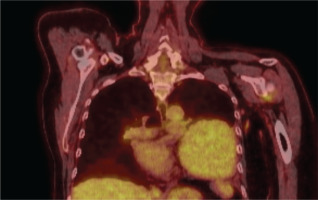
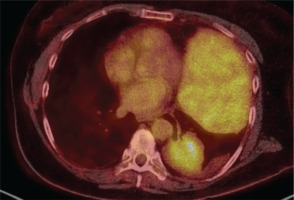
A 64-year-old woman, non-smoker, was referred to hospital with cough and dyspnea gradually deteriorating during the last six months. Her temperature was normal. No rashes and edema of extremities were noticed. Laboratory tests were unremarkable. Oxygen saturation on room air was within normal ranges (SatO2 = 96%). Clinical examination revealed decreased respiratory sounds at the left hemithorax. The chest X-ray (Figure 1) revealed a great opacity at the left middle and lower field. Subsequently, the patient underwent chest CT (Figure 2) which revealed two masses, one in mediastinum which projects within the left hemithorax with maximum diameter at 13 cm and another in left lower lobe with maximum diameter at 5 cm, and also a small amount of ipsilateral pleural fluid. Despite the burden of imaging findings, the bronchoscopy was unremarkable. In pre-operative setting, pulmonary function tests (spirometry and diffuse lung capacity) were within normal limits. The cytological examination of pleural effusion was negative for neoplastic disease. The patient underwent FNB via CT guidance of the mediastinum mass and the biopsy showed thymoma type AB, pT1a (TNM Masaoka-Koga). Staining of antibodies against acetylcholine was positive (32 nm, normal range <0.6), whereas staining of antibodies against Musk was negative. Due to disease staging, the patient was submitted to PET-CT (Figures 3 and 4) which showed a medium FDG uptake (SUVmax = 4.6) to the solid mass of pre-vascular space and a higher FDG uptake of SUVmax = 6 to the lesion of the left lower lobe. The FDG uptake of pleural effusion was low (SUVmax = 1.5). Consequently, the mediastinum mass was surgically resected and simultaneously a left lower lobectomy was performed. The biopsy confirmed thymoma type AB and mixed invasive mucinous and non-mucinous lung adenocarcinoma, respectively.
DISCUSSION
Thymoma patients seem to be susceptible to developing extra malignancies; however, the precise mechanism linking thymoma to increased incidence of cancer remains unclear4. An extensive number of following neoplasms have been reported among thymoma survivors, including non-Hodgkin lymphomas (NHL), soft tissue sarcomas, gastrointestinal malignancies, prostate cancer, breast cancer, lung cancer, and skin cancer. NHL and lung cancer are the most commonly established neoplasms following the presence of thymoma3. According to already published data collected from cancer registries, thymoma patients have an increased probability for B-cell non-Hodgkin lymphoma, due to immune disorder occurring from thymoma or its treatment. This immune dysfunction could probably drive to aberrant cell proliferation and solid tumor growth. Several hypotheses have been described in an effort to provide a probable correlation between thymoma and other malignancies. The increased suppressor T-cell activity leads to pronounced natural killer cell function and this fact provides an explanation of raised incidence of solid tumors in thymoma patients. A second scenario proposes that thymoma epithelium may constantly stimulate T-lymphocytes, which subsequently leads to cancer development. However, these hypotheses do not adequately explain the synchronous presence of thymoma with other solid tumors4.
CONCLUSION
Most cases of second neoplasms occur at a later point of time and awareness of thymoma patients is indicated, to permit earlier identification and therapeutic intervention of any subsequent malignancies4. Moreover, additional data and case reports must be collected in order to determine possible biological processes and the precise pathogenetic correlation of concurrent thymomas and lung cancer. The detection of the linking mechanism of both disorders is crucial to achieve prompt intervention and optimal management of these patients.