INTRODUCTION
The COVID-19 pandemic, caused by SARS-CoV-2, started in Wuhan, China in December 2019, and spread rapidly worldwide causing over 6 million deaths by April 20221. Although the disease is mild in most people, the pandemic had a profound effect on societies and brought social and economic life to a standstill. In most countries, this crisis has overwhelmed the capacities of healthcare systems due to increased patient visits to emergency departments and increased need for hospitalizations in common wards and intensive care units2,3. Early recognition, isolation, and management of these confirmed cases are extremely important as approximately 80% of people with COVID-19 have uncomplicated or mild illness4,5.
A considerable percentage of patients require advice if their respiratory status worsens in the second week of illness; there have been anecdotal reports of patients dying at home because they failed to identify the severity of their symptoms6. Remote support and monitoring for COVID-19 patients are crucial so that the patients can recover completely at home when possible and be advised when in-person evaluation is required. This monitoring ensures that patients stay at home when it is safe to do so, avoiding unnecessary exposure of healthcare workers and the use of valuable personal protective equipment. Furthermore, there is evidence in the literature that early hospital admission leads to improved outcomes7.
Primary care tends to focus on medical care and is characterized by the provision of comprehensive, accessible healthcare services by clinicians who are responsible for addressing the vast majority of personal healthcare needs, establishing long-term relationships with patients, and practicing in the context of family and community8. Primary care physicians played a significant role in diagnosing suspected cases, differentiating confirmed COVID-19 patients based on severity and risk factors, guiding treatment at home in accordance with national guidelines, and referring the more severe cases to hospitals9. In addition, the unprecedented worldwide vaccination campaign relies heavily on primary care physicians10.
Primary care in Greece has two main characteristics. First, private primary care services far outweigh governmentfunded services. Second, the primary healthcare system is, in addition to general practitioners (GPs), based to a very great extent on specialized doctors, such as pulmonologists11. Soon after the pandemic crisis started, Greek policies adopted a risk stratification algorithm for COVID-19 cases proposed by the Hellenic Respiratory Society, which was based on case severity and risk factors for severe disease12. This algorithm positively affected the healthcare system and diminished the number of cases that needed hospital assessment.
The aim of the current study is to explore the contribution of private pulmonologists’ Greek network in the primary care of COVID-19 patients and in the vaccination strategy.
METHODS
For the purposes of the study, we constructed a questionnaire that consisted of 28 simple questions using Survey Monkey online survey creator. The questions were grouped into categories, including ways of initial diagnosis, disease severity, ways of assessment, outcome, management, and vaccination.
The questionnaire was administered only to Greek Private Primary Care Pulmonologists (PPCPs), by sharing a web-link using Hellenic Thoracic Society members e-mail database and the email addresses of the Private Social Networking Pulmonologists’ group.
Users could pause the study and roll back at any time without losing its progress. Although the study was anonymous, users could not answer the study more than once through IP address detection. The questionnaire was sent in June 2021, including only the first 3 pandemic waves. Only physicians who responded to all the questions were included in the study.
The questionnaire that was used for the study is shown in Table 1.
Table 1
Questions that were included in the questionnaire used for the study
RESULTS
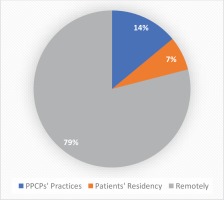
In total, 150 PPCPs completed the study out of 421 registered, a satisfactory percentage of 35%. Most pulmonologists (43%) had their private practices in the capital and the second largest Greek city, and 42% in another town with population more than 25000 people, and 15% in a smaller town. Most responders (57%) have owned their practices for more than 10 years. Although 42.2% of PPCPs examined more than 50 suspected for COVID-19 cases, and 27% more than 100 cases (Figure 1A), most responders (80%) mentioned that the initial testing for COVID-19 disease was not performed in their practices using rapid antigen tests.
Figure 1
A. Percentage of PPCPs that examined more than 100, 51–100 and less than 50 suspected COVID-19 patients. B. Percentage of PPCPs that examined more than 100, 51–100 and less than 50 confirmed COVID-19 patients
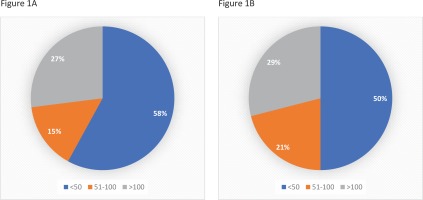
Fifty percent of PPCPs managed more than 50 confirmed COVID-19 patients (via remote or face-to-face assessment), while 28.9% managed more than 100 COVID-19 patients (Figure 1B). At the time of COVID-19 diagnosis, 14% of patients were examined at pulmonologists’ practices, 7% at their residency, and 79% were managed remotely only (Figure 2). Despite quarantine, 28% of COVID-19 patients underwent blood testing and 23% underwent chest X-ray. Less than 5% of positive patients were fully vaccinated for COVID-19 disease at the time of the study. On an average, 60% of patients had mild disease, 24% moderate (findings compatible with pneumonia without hypoxemia), 14% severe (severe pneumonia regarding hospitalization), and 3% critical disease (need for ICU). The most common day of referral to the hospital was between the 6th and 10th day from the onset of the symptoms and the main reason was hypoxemia (72%). Less common reasons included prolonged fever (11%), comorbidities (3%), significant findings from laboratory tests (3%) and increased age (2%).
According to 30% and 55% of pulmonologists, respectively, three medical visits at home and three at private practices were required. Patients who were initially assessed face-to-face, had an increased need for telephone contact with their doctor: 75% were contacted more than 5 times and 37% more than 10 times (Figure 3A). Patients that were managed only remotely also had a remarkably increased need for telephone contact with their doctor: 88% were contacted more than 5 times and 56% more than 10 times (Figure 3B).
Figure 3
A. Average telephone contact with COVID-19 patients (for those assessed at PPCPs practices and patients’ residency). B. Average telephone contact with COVID-19 patients (for those assessed only remotely)

The majority of PPCPs (69.5%) reported a score of 7–10 for how useful the COVID-19 guidelines from the Greek National Public Health Organization were for their daily practice on a scale of 0–10. Besides, most PPCPs (89.5%) reported a score of 7–10 for how useful the COVID-19 guidelines from Hellenic Respiratory Society were for their daily practice on a scale of 0–10. In addition, a substantial proportion of PPCPs (58.1%) reported a score of 7–10 for how useful other COVID-19 guidelines were for their daily practice on a scale of 0–10.
According to PPCPs, 47% of patients remained in quarantine without any intervention, 30% were treated at home, 17% were hospitalized in a common ward, 4% were in ICU, and 2% died.
The majority of PPCPs (78%) provided information for COVID-19 vaccination by telephone to more than 20 patients weekly.
DISCUSSION
Although some countries’ primary healthcare systems responded well to the pandemic and developed viral spread control strategies tailored to primary care13, other countries’ primary care systems reported important issues, such as understaffing, a lack of infection control training, sparse technological support, insufficient collaboration between primary care and secondary or tertiary healthcare facilities, and a lack of emergency response protocols tailored to the needs of a particular population14,15. During the early months of the pandemic, Greek primary healthcare was not as active in COVID-19 strategic planning as it should have been, and health authorities concentrated on hospital readiness as an essential and immediate priority16. However, the Greek experience demonstrated that collaboration between primary and hospital care, led to effective management during the first wave of the pandemic in Greece9.
During the second and third pandemic waves in Greece, most hospitals were organized as referral centers for COVID-19 patients. Emergency departments exhibited significant work overload from confirmed COVID-19 patients, and hospital outpatient clinics were limited as doctors were transferred to COVID-19 departments17. This led to a remarkably increased patient flow to primary care physicians who had to deal with acute and chronic diseases but also with confirmed and suspected COVID-19 cases. As COVID-19 is mainly a disease affecting the lungs, pulmonologists had a cardinal role in patients’ management.
In this study, we explored the role of Greek PPCPs in the COVID-19 pandemic. As was mentioned, the primary healthcare system, in addition to GPs, relies on specialized doctors, such as pulmonologists11. This characteristic is of great importance, as it means that experienced and focused clinicians are managing COVID-19 disease, a medical condition mainly affecting the respiratory system and requiring specific assessment. Our study included the experience from the first three pandemic waves. These waves had distinct characteristics and were probably more challenging for PPCPs, compared to the following waves, which are characterized by delta and omicron variant predominance. More specifically, although confirmed and suspected cases were kept substantially lower due the implementation of a variety of containment and mitigation strategies such as lockdowns18, they were more severe due to the absence of vaccines or low vaccination rates (37% vaccination coverage by the end of June 2021)19. Besides, coronavirus variants, especially the delta variant, were more transmissible and caused more severe disease than previous variants20.
PPCPs also faced several other difficulties, such as low availability of antigen tests and personal protective equipment as they were not provided by the health authorities21. This low availability is reflected by our finding that 80% of PPCPs mentioned that the initial testing for COVID-19 disease was not performed in their practices using rapid antigen tests.
According to the existing literature, despite a variety of obstacles, primary care professionals altered primary care delivery quickly, in order to manage suspected and confirmed cases remotely. Blazey-Martin et al.22 developed an innovative management approach for managing COVID-19 patients remotely by primary care physicians. Frequent conversations with the patients through this program enabled the physicians to follow patients’ symptoms and early detection when a patient was deteriorating. With this approach, they achieved to manage most COVID-19 patients at home, during the first wave of the pandemic22. In another study by Lim et al.13 from Singapore, primary care physicians gave the patients with symptoms of respiratory tract infection 3 to 5 days of home medical leave and highlighted them for subsequent review via an electronic medical records system. Those who reported persistent symptoms were advised to visit the clinic for further workup while those with worsening symptoms were admitted via the public ambulance service or consulted a doctor via the network’s telemedicine mobile application13.
Smyrnakis et al.21 performed semi-structured telephone interviews with 33 primary care professionals, including GPs, general internal medicine specialists, pediatricians, and nurses, recruited from all Greek regions, after the first wave of the pandemic. These professionals followed the guidelines and protocols of the National Public Health Organization (NPHO/EODY). Telephone consultations for patient information and support substituted face-to-face patient contact in most cases21. This was the first qualitative study from Greece to show experiences, ways of management and contribution of the primary care physicians. However, this study did not include primary care pulmonologists.
Of note, most pulmonologists that answered the questionnaire (43%) had their private practices in the capital, Athens, and the second largest Greek city (Thessaloniki) and these results are almost identical to the geographical distribution of Greece’s population, as 42% of the Greek population lives in these two cities23.
According to the study, each PPCP managed a remarkably high number of suspected and confirmed COVID-19 cases. Approximately, one-third of PPCPs examined more than 100 suspected patients and managed more than 100 confirmed cases. This number is relatively high considering the low number of cases in Greece during the first three pandemic waves, as a result of lockdowns and other restrictions.
Most COVID-19 patients (79%) were managed remotely due to the effort to reduce transmission of the disease that was implemented in most European countries24. Despite this, PPCPs examined 21% of their confirmed cases, supporting their patients and reducing the patients’ flow to emergency departments; 14% were examined at their practices and 7% at patients’ residences. Moreover, 28% of COVID-19 patients were offered blood testing and 23% chest imaging, without visiting referral hospitals for COVID-19. In addition, 21% of COVID-19 patients were hospitalized; 17% in common ward, 4% in the ICU and 2% finally died, while most patients (79%) were managed at home, with 30% receiving any kind of treatment. According to PPCPs, the most common day of referral to the hospital was between the 6th and 10th day from the onset of the symptoms, and the main reason was hypoxemia. This is in agreement with the existing literature, which has shown that COVID-19 patients have the potential to rapidly deteriorate about one week after disease onset25. Thus, PPCPs took care of the COVID-19 patients promptly, following the national guidelines for management of COVID-19 patients at home26.
Of note, PPCPs maintained close follow-up of both the patients that were examined and patients managed remotely, with frequent visits and telephone contacts, overcoming the quarantine difficulties. This was another factor contributing to the successful management of these patients, as it has been reported that, in addition to strong primary health care systems, close follow-up of patients is associated with optimal continuity of healthcare and better outcomes27.
Interestingly, the majority of PPCPs reported a score of 7–10 for how useful the COVID-19 guidelines from the Greek National Public Health Organization, from Hellenic Respiratory Society and other COVID-19 guidelines were for their daily practice on a scale of 0–10. Similar to our study, it has been reported in other countries that the national guidelines are well known, and the majority of physicians consider them very relevant, simple to follow, reliable, and beneficial. Most of the physicians have reported using the recommendations to support their own clinical judgment, believing that these recommendations increased confidence while making clinical decisions since they were a consistent, dependable source of evidence-based advice28.
The majority of COVID-19 cases were unvaccinated (95%), and this probably reflects the efficacy of vaccines before the omicron variant predominance or the low vaccine coverage of the population29. Vaccinations were only available in public hospitals in Greece during the first semester, and private doctors could only advise their patients on the need for and efficacy of vaccination30. There was an increased awareness of information by patients, as 78% of PPCPs provided this information by telephone for more than 20 patients weekly. It is critical that patients received individualized vaccination advice that is more efficient because it is based on the doctor-patient relationship31. Primary care physicians are at the forefront of communicating with the community, and have been highly influential in the uptake of vaccines in previous pandemics32.
The Health Information Exchange (CRISP) in Maryland, USA, has established a set of data for each primary care practice to select patients who are suitable for the COVID-19 vaccination based on demographics and chronic illness, as well as patient names for focused outreach. Primary care physicians were educated and trained on how to use data, and new tools for community outreach were developed to supplement primary care’s efforts33. In the same line, PPCPs supported vaccination centers and, most importantly, offered consultation to their patients, reducing vaccination hesitancy.
Strengths and limitations
To the best of our knowledge, this is the first study to analyze the contribution of PPCPs to the COVID-19 pandemic. One advantage of the study is that it was accessible to most target physicians, meeting them where they were. Another advantage is that there were no cost-based geographical restrictions. However, there are some limitations. The main limitation is that its results are based on different databases/ patients’ records from several pulmonologists and not from a centralized healthcare databases/centralized electronic health database, and the results cannot be checked for their integrity34. Besides, as the study was anonymous, we cannot correlate the number of COVID-19 patients managed by PPCPs with the number of cases/patients in each geographical area. As a result, the findings indicate, at best, an increase in the workload of PPCPs. Another limitation is that the questionnaire in this study has not been validated as a tool since this was not the aim of the study.
CONCLUSIONS
Our study shows that PPCPs in Greece offered high quality, specialized, frequent and integrated support for COVID-19 patients, overcoming the difficulties of containment and mitigation strategies and the limited access to personal protective equipment and antigen testing. This probably contributed to reducing the work overload of emergency departments during the first three waves. Furthermore, by providing individualized advice on vaccination, they supported national efforts for COVID-19 vaccination.