INTRODUCTION
The ongoing pandemic of 2019 novel coronavirus disease (COVID-19) has affected every region around the world and continues to impact lives and healthcare systems globally1-3. The causative virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first identified in China on 7 January 2020, but has spread rapidly across the world causing a global public health crisis over the past three years4-8. About 678 million confirmed cases and over 6.7 million deaths due to COVID-19 have been registered worldwide. In Greece, SARS-CoV-2 has resulted in more than 5.5 million cases of COVID-19 and more than 34700 deaths up to February 2023. Despite advances in treatment and implementation of vaccination policies by national authorities, we are facing the ‘SARS-CoV-2 variants of concern’ era of the pandemic with 19712 confirmed cases and 964 admissions of patients with COVID-19 in hospitals in January 2023, in Greece. Epidemiological data from patients hospitalized with COVID-19 during the fourth and fifth waves of the pandemic have been published in several countries9-13; yet, to the best of our knowledge, nationwide data in Greece remain limited. The aim of our study was to register baseline characteristics, clinical and radiological features, laboratory data, treatment modalities and outcomes of a registry of patients hospitalized with COVID-19 across Greece. Our study represents the first epidemiological report nationwide from Greece during the fourth and fifth waves of the COVID-19 pandemic. We provide scientific evidence that specific disease prognosticators derived from imaging and laboratory tests represent reliable markers leading to timely therapeutic interventions.
METHODS
In this observational, prospective study between 12 November 2021 and 8 June 2022, we enrolled consecutive hospitalized patients with COVID-19 in seven reference hospitals in South, Central and North Greece, including Department of Respiratory Medicine, University Hospital of Patras, 2nd Respiratory Medicine Department, ‘Attikon’ University Hospital, National and Kapodistrian University of Athens, 1st Respiratory Medicine Department, ‘Sotiria’ Chest Hospital, National and Kapodistrian University of Athens, 4th Respiratory Medicine Department, ‘Sotiria’ Chest Hospital, Athens, Respiratory Medicine Department, University of Ioannina, 5th Respiratory Medicine Department, ‘Sotiria’ Chest Hospital, Athens, and COVID-19 Clinic, General Hospital G. Papanikolaou, Aristotle University of Thessaloniki.
Diagnosis of COVID-19 was established with a positive real-time reverse transcriptase polymerase chain reaction (RT-PCR) of an upper respiratory nasopharyngeal swab. Subsequently, we recorded demographic data, radiology features and laboratory tests including parameters of complete blood count, ferritin, lactate dehydrogenase (LDH) and d-dimer. Comorbidities, duration of hospitalization, maximum fraction of inspired oxygen (FiO2), as well as outcome of hospitalization were also recorded. Maximum FiO2 during hospitalization, as well as Charlson Comorbidity Index (CCI) on admission (range: 0–37) were correlated with disease severity. Increased values of CCI were indicative of reduced estimated 10-year survival14,15.
Statistical analysis
With regard to baseline data, summary descriptive statistics were generated with categorical data displayed as frequencies and percentages. Continuous data were expressed as mean ± standard deviation (SD) or median with 95% confidence interval (95% CI) following Kolmogorov-Smirnov test for normality. Median values of complete laboratory tests were calculated, as in all cases Kolmogorov–Smirnov test for normal distribution rejected normality. Mann-Whitney test was used to assess differences in CCI on admission and maximum FiO2 during hospitalization between subgroups of patients separated by the median value of parameters under investigation (high and low subgroup). A p<0.05 was considered statistically significant.
RESULTS
Clinical and radiological data
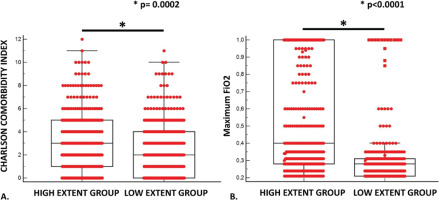
Baseline characteristics of this cohort are presented in Table 1. A total of 1019 consecutive cases were included and analyzed; 55.1% of patients were male, median age of 67 years (95% CI: 65.7–69) and 55.8% of them were fully vaccinated against SARS-CoV-2. Interestingly, 57.2% of patients were non-smokers. With regard to clinical symptomatology on admission, dyspnea (41.4%), fever (40.8%), cough (39.4%) and general fatigue (30.3%) were the predominant features, while 13.2% and 9.7% experienced headache and anosmia, respectively. Radiological features were similar in the vast majority of patients and included interstitial infiltrates bilaterally in chest X-ray (51.5%) and findings consistent with organizing pneumonia and non-specific interstitial pneumonia. More specifically, consolidation and ground glass opacities with no distinct predominance were noticed in chest computed tomography (CT) performed in patients presented with PaO2/FiO2 <200 at any time during their hospitalization (78.6%) (Table 2). Patients with increased extent of consolidation and ground glass opacities in chest CT (>10–25%) presented with more severe disease compared to the low extent group (<10%) as indicated by both CCI on admission (3; 95% CI: 2–3 vs 2; 95% CI: 1–2, p=0.0002, respectively) (Figure 1A) and MaxFiO2 (0.40; 95% CI: 0.35–0.40 vs 0.28; 95% CI: 0.24–0.28, p<0.0001, respectively) (Figure 1B). Arterial hypertension was the most common comorbid disease (45.0%), while 21.4%, 11.5% and 10.9% of patients were previously diagnosed with diabetes mellitus, cancer and coronary heart disease, respectively. Interestingly, chronic obstructive pulmonary disease (COPD) and asthma as comorbidities were recorded in a minority of patients with a frequency of 9.7% and 6.0%, respectively (Table 3). Most of hospitalized patients were administered with the standard-of-care therapeutic modality, including dexamethasone (78.7%) – in case of respiratory failure – for up to 10 days or until discharge from hospital, whichever occurred first, and remdesivir (78.2%) for up to 5 days. Biologics including anti-IL6 (tocilizumab) and oral selective Janus kinase 1/2 inhibitor (baricitinib) were administered in 79 patients (7.8%) and 70 patients (6.9%), respectively, while only 0.5% and 0.7% received anti-IL1r (anakinra) and convalescent plasma, respectively. Prophylactic low-molecular weight heparin was given in 81.6% of patients. More than 50% of patients received antibiotics based on clinician’s judgment for bacterial co-infection (Table 4). Median time of hospitalization was 8 days (95% CI: 7–8). Seventy-two (7.1%) of our patients were admitted in an Intensive Care Unit [median age: 68.5 years (95% CI: 65.2–71), median CCI: 4 (95% CI: 3–4)] and 154 died (15.1%) [mean age: 73.2 ± 9.2, median CCI: 5 (95% CI: 4–8)].
Table 1
Baseline characteristics of patients enrolled in the study (N=1019)
Table 2
Clinical and radiological features on admission of patients enrolled in the study (N=1019)
Table 3
Comorbidities of patients enrolled in the study (N=1019)
Table 4
Therapeutic compounds administered to the study population (N=1019)
Figure 1
A) Median Charlson comorbidity index on admission was significantly higher for patients with increased extent of consolidation and ground glass opacities in chest CT (>10–25%) (3; 95% CI: 2–3) compared to the low extent group (2; 95% CI: 1–2) (p=0.0002); B) Maximum FiO2 during hospitalization was significantly higher for patients with increased extent of consolidation and ground glass opacities in chest CT (>10–25%) (0.40; 95% CI: 0.35–0.40) compared to the low extent group (0.28; 95% CI: 0.24–0.28) (p<0.0001)
Laboratory data
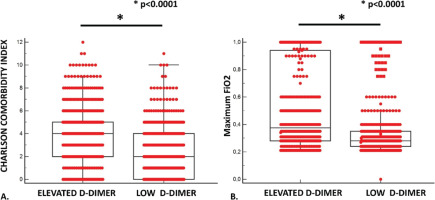
Laboratory data of this cohort are presented in Table 5. Lymphopenia (<1200/μL) was common, recorded in 62.7% of hospitalized patients with median values of 1030/μL (95% CI: 980–1070). Consequently, neutrophil to lymphocyte ratio (NLR) was calculated with a median value of 4.42 (95% CI: 4.1–4.8). Ferritin levels (>90 ng/mL) were also elevated in most of patients (62.6%) with a median value of 282.8 (95% CI: 252.7–303.5). Increased LDH levels (>245I U/mL) were recorded in the majority of the cohort (59.8%) with a median value of 269 (95% CI: 260–277). Elevated d-dimer levels (>0.5 ng/mL) were noticed in 657/1019 (64.5%) of hospitalized patients. Remarkably, patients with high neutrophil to lymphocyte ratio (≥4.42) suffered from more severe disease as shown by significantly increased CCI on admission (4; 95% CI: 3–4 vs 3; 95% CI: 2–3, p<0.0001, respectively) (Figure 2A) and MaxFiO2 (0.35; 95% CI: 0.35–0.40 vs 0.28; 95% CI: 0.28–0.28, p<0.0001, respectively) (Figure 2B). Finally, patients with increased d-dimer (≥0.74 μg/mL) demonstrated also severe disease compared to the low d-dimer group (<0.74 μg/mL), as assessed by both CCI on admission (4; 95% CI: 4–4 vs 2; 95% CI: 2–2, p<0.0001, respectively) (Figure 3A) and MaxFiO2 (0.38; 95% CI: 0.35–0.40 vs 0.28; 95% CI: 0.28–0.28, p<0.0001, respectively) (Figure 3B).
Table 5
Laboratory tests on admission of patients enrolled in the study
Figure 2
A) Median Charlson comorbidity index on admission was significantly higher for patients with high neutrophil to lymphocyte ratio (≥4.42) (4; 95% CI: 3–4) compared to patients with low neutrophil to lymphocyte ratio (<4.42) (3; 95% CI: 2–3) (p<0.0001); B) Maximum FiO2 during hospitalization was significantly higher for patients with high neutrophil to lymphocyte ratio (≥4.42) (0.35; 95% CI: 0.35–0.40) compared to patients with low neutrophil to lymphocyte ratio (<4.42) (0.28; 95% CI: 0.28–0.28) (p<0.0001)
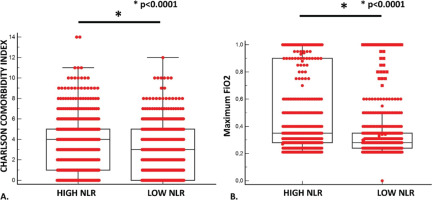
Figure 3
A) Median Charlson comorbidity index on admission was significantly higher for patients with elevated d-dimer (≥0.74 μg/mL) (4; 95% CI: 4–4) compared to patients with low d-dimer (<0.74 μg/ mL) (2; 95% CI: 2–2) (p<0.0001); B) Maximum FiO2 during hospitalization was significantly higher for patients with elevated d-dimer (≥0.74 μg/mL) (0.38; 95% CI: 0.35–0.40) compared to patients with low d-dimer (<0.74 μg/mL) (0.28; 95% CI: 0.28–0.28) (p<0.0001)
Adverse events
Adverse events during hospitalization are presented in Table 6. In particular, 144 patients (14.1%) presented with new onset infection during hospitalization, while bleeding with hemodynamic instability and acute kidney injury occurred in 11.8% and 8.8% of patients, respectively. Moreover, only 37 patients (3.6%) presented with thromboembolic events (pulmonary embolism or deep vein thrombosis), while cardiovascular events occurred in 3.3% of patients.
DISCUSSION
This cohort was the first epidemiological study across Greece of hospitalized patients with COVID-19 during the fourth and fifth waves of the pandemic. Elicited conclusions from this multicenter registry further verified evidence from previous studies with regard to epidemiological characteristics, clinical and radiological features, laboratory data, treatment modalities, adverse events and outcomes. More specifically, prevalence was increased among middle-aged males, non-smokers and patients with cardiovascular risk factors (45% and 21.4% had arterial hypertension and diabetes mellitus as comorbid disease, respectively)16-19. Interestingly, almost half of hospitalized patients (44.2%) were unvaccinated for SARS-CoV-2, a slightly different finding compared to previous waves of pandemic. Our study group has shown that in the delta variant era, 71.5% of patients hospitalized due to COVID-19 in Greece were unvaccinated against SARS-CoV-22. Dyspnea, fever and cough were noticed more commonly with regard to clinical symptomatology, while bilateral interstitial infiltrates were present in 51.5% of patients’ chest X-rays. Combination of dexamethasone and remdesivir were vastly applied in the context of current WHO guidelines.
Beyond the aforementioned highly reproducible epidemiological data, our study revealed some interesting observations with regard to clinical applicable biomarkers of COVID-19 severity in hospitalized patients. First, the high extent group of consolidation and ground glass opacities in chest CT (>10–25%) exhibited more severe disease compared to the low extent group (<10%) as shown by both CCI on admission and MaxFiO2. In order to quantify the extent of SARS-CoV-2 infection, radiograph scoring depending on the extent of consolidation or ground-glass opacities in chest CT was used from the beginning of the pandemic20-22. Moreover, increased NLR (≥4.42) could be used in everyday clinical practice as a biomarker of disease severity, as it was proven reliable in discrimination between severe and non-severe cases based on CCI on admission and MaxFiO2. This finding further validated previous research for the negative impact of elevated NLR on patients with SARS-CoV-2 infection. NLR has been proven to be a marker of inflammation that could be correlated with mortality in patients with miscellaneous cardiovascular diseases or sepsis23,24. For patients with SARS-CoV-2 infection, NLR has been characterized as an independent risk factor for severe disease25-27. Elevated NLR has been associated with dysregulated expression of inflammatory cytokines, aberrant increase of irregular low-density neutrophil and the upregulation of genes with crucial role in lymphocyte apoptosis pathway, provoked by the pathogenetic mechanisms of SARS-CoV-2 infection28. Finally, increased d-dimer levels were also associated with worse clinical outcomes, as indicated by CCI on admission and MaxFiO2. It is well documented that even though d-dimer is helpful in detecting thromboembolic events, elevated levels have been correlated with malignant diseases, chronic liver diseases, postoperative conditions, pregnancy and inflammation. Despite the fact that d-dimer represents a biomarker with low specificity and sensitivity, a dynamic association between elevated d-dimer levels with COVID-19 severity has been widely reported29-33. Patients with COVID-19 and comorbid diseases are led into a vicious infectious circle of life and are substantially associated with significant morbidity and mortality and require scrupulous management34. CCI that was used to define severity of disease is considered the gold standard to assess comorbid risk in clinical research15.
Limitations
Our study presents some limitations. This registry was not scheduled to provide mechanistic data and as it was a hospital-based epidemiological study with patient characteristics; quality of data is characterized by sampling bias. Finally, conclusions of long-term follow-up assessment were not feasible.
CONCLUSIONS
Collectively, this study highlighted real-life data of hospitalized patients due to COVID-19 during fourth and fifth waves of pandemic across Greece. To the best of our knowledge, this is the first nationwide epidemiological report for Greece for that period of the pandemic. Our findings are in line with previous published data indicating a global clinical, laboratory and radiological appearance of COVID-19. Combination of extent of radiological features, neutrophil to lymphocyte ratio (NLR) and d-dimer may represent reliable disease prognostic factors leading to timely therapeutic interventions. Future nationwide larger updated epidemiological studies are greatly anticipated.