INTRODUCTION
Smoking among healthcare professionals (HCPs) is a serious issue for occupational health and for health promotion. Although healthcare workers are aware of the dangers of smoking1, smoking is not uncommon among them. However, their intervention is critical in promoting healthy behavior and preventing smoking. HCPs are considered to play three roles in society: being role models, acting as caregivers, and providing education to their patients2. Their smoking behavior is directly related to knowledge, attitudes and counseling practices against smoking3 and is very important in the management of patients’ smoking habit as it may limit HCPs’ ability to intervene with their patients2.
In recent years, HCPs are also faced with another phenomenon, Burnout Syndrome (BS). BS was first described in 1974 by Herbert Freudenberger as the response to long-term stress due to adverse conditions at work4. Today, BS is included in the 11th Revision of the International Classification of Diseases (ICD-11) as an occupational phenomenon (not a disease) and a syndrome resulting from chronic stress created in the workplace, which is not adequately treated5. BS is more common in physicians than in the general population and can be seen at any stage of their career6. Workplace factors seem to play a dominant role in its occurrence7. Excessive workload, working ≥40 hours per week, conflict between work and family obligations, loss of support from colleagues, low pay, leadership in the workplace, high goals which sometimes cannot rest on a proper foundation, staff shortages, lack of a trusted partner, excessive alcohol consumption, and disturbed sleep quality have been associated with BS among physicians7. BS is a clinically significant condition associated with reduced quality of life, disturbances in physician health, and decreased patient satisfaction due to reduced quality of care8. It is also associated with an increased risk of traffic accidents9, a 25% increased likelihood of alcohol abuse/dependence10, twice the risk of suicidal ideation11, and twice the risk of medical error12.
On 11 March 2020, the World Health Organization (WHO) declared COVID-19 a global pandemic in the context of which restrictive measures were imposed to prevent its spread. Both the pandemic and the restrictive measures disrupted people’s daily lives and often led to changes in lifestyle behaviors. Regarding smoking, some studies report that it increased during the COVID-19 pandemic13 and others that it decreased14. During a crisis period, such as the pandemic, people tend to exhibit irrational and inappropriate behaviors due to negative emotions, and increased cigarette consumption has been shown to be associated with high levels of psychological stress15. On the other hand, the awareness of the relationship between tobacco use and the worsening of COVID-19 symptoms16, the absence of daily socialization, and reduced access to tobacco products17 due to the restrictive measures, probably led many people to reduce cigarette consumption. During the crisis of the COVID-19 pandemic, HCPs have been working non-stop and as a result they report physical and mental exhaustion. The prevalence of BS among HCPs during the pandemic appears to be as high as 55% and is related to the time spent at the workplace, the number of COVID-19 positive patients who receive treatment, and the number of COVID-19 positive patients who lose their lives18. Research on BS and smoking is limited19.
The purpose of the present study is to investigate the change in the smoking habits of HCPs during the COVID-19 pandemic, to determine BS among HCPs due to the COVID-19 pandemic, and to determine its correlation with smoking.
METHODS
A descriptive, cross-sectional study was performed based on a sample of 278 HCPs in the area of Kozani city in Greece. The study took place from March to May 2022. For its implementation, approval was received from the Postgraduate Program in Management of Aging and Chronic Diseases of the School of Social Sciences of the Hellenic Open University, and all principles of research ethics (Declaration of Helsinki, 1975) concerning personal data were observed. An electronic questionnaire was used. The electronic questionnaire, due to the restrictions imposed in the context of the pandemic, was promoted to HCPs profiles in social media via snowball sampling and was also promoted by the Kozani Medical Association to its members via email. Participation was voluntary, maintaining anonymity, since before their participation, the social media users were informed in detail, on each platform, about the purpose of the study.
Questionnaire
The first part of the questionnaire consisted of questions related to the sociodemographic and work characteristics of the participants. The second part consisted of questions on their health status and the people they live with, whether their health is at risk due to their work, and their views on smoking and COVID-19. The Copenhagen Burnout Inventory (CBI) was used for occupational burnout. The CBI was created by Kristensen et al.20 with the main advantage that it can assess burnout in a wide range of occupations. It can predict future sickness absence, sleep problems, pain medication use, and intention of smoking cessation20. A Greek study showed that it is a valid tool with high internal consistency, and can be used in the assessment of BS in the Greek population21. The CBI consists of 19 items which evaluate three components or subscales.
Personal Burnout
Assessed by questions 1–6:
1. How often do you feel tired?
2. How often are you physically exhausted?
3. How often are you emotionally exhausted?
4. How often do you think: ‘I can’t take it anymore’?
5. How often do you feel worn out?
6. How often do you feel weak and susceptible to illness?
Work-related Burnout
Assessed by questions 7–13:
7. Is your work emotionally exhausting?
8. Do you feel burnt out because of your work?
9. Does your work frustrate you?
10. Do you feel worn out at the end of the working day?
11. Are you exhausted in the morning at the thought of another day at work?
12. Do you feel that every working hour is tiring for you?
13. Do you have enough energy for family and friends during leisure time?
Client-related Burnout
A state of prolonged physical and psychological exhaustion which is related to the cooperation-association of the individual with the client, assessed by questions 14–19:
14. Do you find it hard to work with clients?
15. Do you find it frustrating to work with clients?
16. Does it drain your energy to work with clients?
17. Do you feel that you give more than you get back when you work with clients?
18. Are you tired of working with clients?
19. Do you sometimes wonder how long you will be able to continue working with clients?
The score in each subscale is obtained as an average from the scale of responses: 0, 25, 50, 75 and 100, where a higher mean indicates higher burnout. Finally, the smoking behavior section included questions about individual and family smoking history before and during the COVID-19 pandemic. The Fagerström test for nicotine dependence (FTND) scale was also used. The FTND is used internationally to assess smoking dependence and identify the patient’s smoking status22. In clinical practice, the Fagerström scale can be used for the selection of the treatment regimen during smoking cessation23.
Statistical analysis
Data analysis was carried out using SPSS software (IBM Corp. Released 2021, IBM SPSS Statistics for Windows, v.28.0, Armonk, NY: IBM Corp.). Frequency distributions of the 278 HCPs’ particular characteristics, work and experience were calculated. The graded responses to the questions for each scale, on the pandemic, occupational burnout (CBI), and FTND, were compared using the χ2 method (homogeneity) and the estimation of 95% confidence intervals (95% CIs). The CBI subscales were compared hierarchically using the non-parametric Friedman method. Their scores were checked for their distribution with the Blom method (QQ plot) without detecting asymmetry, while the χ2 method was used to determine correlation with the characteristics of the participants and smoking habits or change. The McNemar method was used to determine the change in smoking habits from the period before the COVID-19 pandemic to the current period. Finally, multiple linear regression was applied to correlate the burnout of the 278 HCPs with their particular characteristics, current smoking habit, and nicotine dependence. The level of significance was set at 0.05.
RESULTS
The majority of the study participants (71.6%) were women (Table 1), the mean age of all participants was 42.0 years (range: 23–73), and 60.8% were married. In terms of their education, about half of them (48.6%) stated that they held a postgraduate degree (PhD, MSc). In their professional capacity almost half of them (53.6%) were physicians (including a dentist). From the percentage distribution of working years, 24.5% had worked for >20 years while only 2.5% had worked for <2 years.
Table 1
Basic characteristics of health professionals who participated in the study
Figure 1 presents, in a hierarchical arrangement, the frequencies of the responses to six questions related to health status and the perception of the risk of COVID-19 infection. All the participants (100.0%) stated that they are at risk of coming into contact with the SARS-CoV-2 virus in their workplace, 80.2% expressed their belief that smokers manifest severe disease compared to non-smokers if infected with SARS-CoV-2, and 50.0% believe that smokers are at higher risk of becoming infected. At a low frequency, they also stated that they live with people at high risk of COVID-19 severe disease (19.8%), that they have some chronic health problems (16.9%), and that if they are infected by the SARS-CoV-2 virus, they will manifest the disease with higher severity (15.8%).
Figure 1
Responses to six questions regarding health and risk perceptions for COVID-19 infection of healthcare professionals

CBI scores are presented in Table 2. Levels close to 100 define a very high degree of BS. The average scores indicate moderate or low levels of burnout, while the average Personal Burnout score of 53.8 ± 18.4 was significantly higher than that of Work-related Burnout (49.2 ± 17.4) and Client-related Burnout (29.9 ± 18.0) (p<0.001). Their reliability was 0.795–0.880 (excellent). However, a very small percentage of HCPs presented high/severe burnout in all three subscales: 14.0% in Personal Burnout, 8.6% in Work-related Burnout, and only 1.8% in Client-related Burnout (results not shown).
Table 2
Subscale levels of the Copenhagen Burnout Inventory (CBI) of the health professionals who participated in the study
| Subscales of burnout | Mean* | SD | Median | Min | Max | Cronbach α |
|---|---|---|---|---|---|---|
| Personal | 53.8 | 18.4 | 54.1 | 4.2 | 100.0 | 0.881 |
| Work-related | 49.2 | 17.4 | 48.2 | 3.6 | 100.0 | 0.815 |
| Client-related | 29.9 | 18.0 | 29.1 | 0.0 | 87.5 | 0.827 |
Table 3 shows the responses to questions on the smoking habits of HCPs before the COVID-19 pandemic and during the current period. There is a significant decrease in smokers from 60.1% in the pre-pandemic era to 43.2% in the current period (p<0.001). However, their detailed classification into subgroups shows a non-significant change in smokers (on a daily basis for ≥3 months) from 32.1% to 30.7%, and in those who remained non-smokers from 40.1% to 40.9% (p>0.05). Median consumption was estimated at 10 cigarettes/day and duration 15.0 years of smoking; 61.9% of HCPs reported that their parents smoked or smoke, 30.9% stated that someone else smokes in their household, and 28.4% reported smoking at work. Also, 5.4% of those who did not smoke before the pandemic thought about starting smoking but did not do so, while 17.4% of those who had stopped smoking before the pandemic thought about and started smoking during the pandemic. Although there was a significant decrease in the smoking habit of HCPs, it seems that this reduction was not related to the particular characteristics of the participants (gender, age, family status, education level, financial difficulties, working years, responsible position, and job sector).
Table 3
Smoking habits of healthcare professionals of the study, before the COVID-19 pandemic and during the current period
In Figure 2, a smaller reduction in smokers is observed among HCPs who are physicians or nurses compared to the rest (-16.2% and -16.1% versus -25.5%, p>0.05). Likewise, 27.7% reported that they smoke more, 52.7% that they smoke the same, and 19.6% that they smoke less than usual. Regarding changes in smoking cessation, 57.1% thought about stopping before the COVID-19 pandemic and only 42.9% made an effort. Similarly, 46.2% thought about stopping smoking during the COVID-19 pandemic (26.5% made an effort). In addition, 20.7% consider that their ability to quit smoking has increased during the pandemic era. FTND scores were low, 3.5 ± 2.5, indicating a low degree of dependence. Also in the current period, a significantly higher percentage of the non-smoker HCPs compared to the smokers, advise patients to stop smoking (χ2 test: 87.3% vs 70.8%, p=0.001).
Figure 2
Smoking habit related to the different healthcare professions, before the pandemic and during the current period
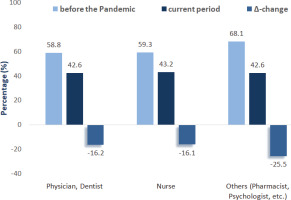
Table 4 shows the correlation of smoking before the pandemic and during the current period, with burnout levels. A significantly smaller reduction in smokers was found among those experiencing high/severe burnout versus those experiencing low or moderate burnout (-4.2% vs -15.2% and -23.7%, p=0.014).
Table 4
Correlation of health professionals’ smoking habits before the pandemic and during the current period with levels of burnout
Finally, Table 5 presents at a multivariable level, through multiple linear regression, the overall correlation of occupational burnout with the special characteristics of the HCPs, current smoking habit and nicotine dependence. Personal burnout appears to be significantly associated with being a physician (β=5.62, p=0.038), increased financial difficulties (β=4.87, p=0.015) and working in the public sector (β= -7.24, p=0.005). Work-related Burnout is significantly associated with younger age of HCPs (β= -0.45, p=0.039), more years of work (β=2.56, p=0.050) and working in the public sector (β= -6.20, p=0.011). Client-related Burnout is also significantly associated with being a physician (β=6.13, p=0.023) and working in the public sector (β= -5.41, p=0.033).
Table 5
Multiple linear correlation of healthcare professionals’ burnout with their characteristics, current smoking habit, and nicotine dependence
| Variables (scales)* | Burnout | |||||
|---|---|---|---|---|---|---|
| Personal | Work-related | Client-related | ||||
| β | p | β | p | β | p | |
| Gender (1: male, 2: female) | 3.90 | 0.143 | 1.73 | 0.494 | 0.18 | 0.946 |
| Age (years) | -0.34 | 0.141 | -0.45 | 0.039 | -0.10 | 0.666 |
| Marital status (1: single/divorced, 2: married) | 4.78 | 0.064 | 3.64 | 0.137 | 2.41 | 0.348 |
| Education level (1: Secondary education, Gymnasium, Lyceum, Institute of Vocational Training, 2: Tertiary Education, 3: PhD/MSc) | -1.12 | 0.530 | 0.03 | 0.984 | 1.96 | 0.273 |
| Health profession (1: Nurse, pharmacist, psychologist etc., 2: Physician/dentist) | 5.62 | 0.038 | 3.33 | 0.194 | 6.13 | 0.023 |
| Financial difficulties (1: not at all, 2: some, 3: several) | 4.87 | 0.015 | 2.92 | 0.124 | 3.71 | 0.062 |
| Employment years (1: <2, 2: 2–5, 3: 6–10, 4: 11–15, 5: 16–20, 6: ≥21) | 1.41 | 0.303 | 2.56 | 0.050 | 0.51 | 0.710 |
| Responsible position (1: no, 2: yes) | 2.48 | 0.328 | 2.78 | 0.248 | 1.86 | 0.460 |
| Work sector (1: Public sector, 2: Private sector) | -7.24 | 0.005 | -6.20 | 0.011 | -5.41 | 0.033 |
| Chronic health problem (1: no, 2: yes) | -2.20 | 0.467 | -2.57 | 0.372 | 1.98 | 0.512 |
| Current smoking status (1: no, 2: yes) | -0.82 | 0.824 | 3.83 | 0.273 | -0.95 | 0.795 |
| FTND scale (0: non-smoker, 1: low, 2: low to moderate, 3: moderate, 4: high) | 2.27 | 0.143 | -1.01 | 0.493 | -1.09 | 0.479 |
| R2 adjusted | 0.060 | 0.042 | 0.021 | |||
DISCUSSION
The present study aimed to assess the change in conventional cigarette smoking habits of HCPs during the pandemic and research the factors affecting that change, placing particular emphasis on its association with occupational burnout. Therefore, according to the findings: 1) a significant reduction in the smoking habits of HCPs was found; 2) the reduction of smokers was significantly smaller among those experiencing high/severe Work-related Burnout compared to those experiencing low or moderate Workrelated Burnout (p=0.014), a result that inextricably links the smoking habit with increased Work-related Burnout; and 3) current smoking habit and nicotine dependence did not have a significant correlation with any of the three forms of burnout, while being a physician, years of work, and working in the public sector, determined higher Personal or Work-related Burnout.
During the course of our research, no other study was found that links BS with change in smoking habits in HCPs during the COVID-19 pandemic. More generally, however, several studies have shown that the COVID-19 pandemic has caused changes in the smoking habit of the population at large. The results of the present study showed a significant decrease in HCP smokers during the pandemic, from 60.1% before the pandemic to 43.2% during the current period (p<0.001). In our study, the percentage of smokers who stopped smoking is higher than that found in an Italian study of the general population, where 5.5% were reported stopping or reducing smoking24. The results of our study are in contrast to those of Jackson et al.25, in the general population in the UK, who report a significant increase in smoking prevalence in 2019–2020 compared to 2018–2019 (24.7% versus 0.0%, respectively). While there has been a significant decrease in smokers, unfortunately many HCPs continue to smoke (43.2%). The percentage of HCPs in our study who are smokers during the current period is higher than that in the general population (43.2% versus 27.5%)26, higher than an earlier Greek study showing that 38.6% of HCPs were smokers27 and lower than the percentage found by Vagropoulos et al.28 in a Greek hospital, where 50% of HCPs were smokers, with 32% of non-smokers being ex-smokers. Moreover, the results of the present study reveal a similar percentage of smokers to Chinese (45%) and Japanese (43%) HCPs, but a higher percentage than in Kuwait (38%) and France (34%)29. Despite the significant decrease of smokers in our study, no correlation was found between this reduction and the special characteristics of the participants. There was a marginally non-significant higher decrease of smokers among married participants (-20.8% versus -13.0%, p=0.095) and a smaller reduction among physicians and nurses versus others (-16.2% and -16.1% versus -25.5%, p>0.05). More generally, a significant correlation is reported between profession and smoking behavior30. Physicians working in public hospitals smoke more30 and nursing staff present the highest percentage of smokers29,30. Other studies have found that marital status affects smoking habit, with unmarried HCPs being more likely to smoke29.
Concerning smokers during the current period, it appears that 27.7% of participants smoke more than previously, 52.7% smoke the same amount, and 19.6% smoke less. A similar study in Turkey showed that during the pandemic smoking frequency increased in 22.4% of HCP smokers and decreased in 20.3%31, while in Italy and Israel, 43% and 35% of HCPs smoked more, respectively32. The mean FTND score in our study was low (3.5 ± 2.5), indicating a low degree of dependence, while only 7.3% presented a high degree of dependence. The study by Cofta and Staszewski30, on the contrary, revealed a strong nicotine dependence among HCPs. Unfortunately, in the present study, as in previous ones, it appears that the smoking behavior of HCPs affects their work, as a significantly higher percentage of non-smoker HCPs compared to smokers advise patients to stop smoking27,29.
Concerning occupational burnout, the mean scores of the CBI subscales indicated moderate/low levels of BS, with Personal Burnout scoring significantly higher than the others (Work-related and Client-related Burnout) (p<0.001). A very small percentage of HCPs presented high/severe burnout in all three subscales, results that do not match other studies indicating a BS prevalence of up to 55% among HCPs during the COVID-19 pandemic18. However, the low rate of Client-related Burnout matches other international studies using the CBI33. It also seems that being a physician, years of work, and working in the public sector, result in higher levels of Burnout, contrasting with studies arguing that BS is correlated with gender and marital status7 but agreeing with the results of Αfonso et al.7 who found that workplace rather than personal factors weighs more heavily in the occurrence of BS. Our study also revealed that Work-related Burnout is significantly associated with younger age of HCPs (β= -0.45, p=0.039) and more years of work (β=2.56, p=0.050). In the literature, it seems that the relationship of burnout with age has been inconsistent. Studies have found that younger employees had higher burnout than other age groups34. On the other hand, studies of Finnish employees reported a U-shape association between age and burnout, and a study among Swedish employees reported higher levels of burnout among older workers34.
Finally, the present study found a significantly smaller reduction in smokers among those experiencing high/severe Work-related Burnout versus those experiencing low or moderate levels (p=0.014), a result that inextricably links smoking habit with increased Work-related Burnout. There is limited study investigating the relationship between BS and smoking19. Moreover, various studies have used different instruments or definitions of BS, something which only assists in inductive comparisons35. The results of our study are in agreement with those of several studies which found that smoking is correlated with BS. Smoking habit has been observed to be an important prognostic indicator for higher BS scores19. Smoking appears to be negatively correlated with all dimensions of occupational burnout35. Smokers also present a higher frequency of occupational burnout compared to non-smokers36. These results demonstrate that there is a correlation between smoking habit and burnout. On the other hand, other studies have not found any correlation between smoking and BS37.
Limitations
Stratified random sampling could not be applied to this observational study, with the result that the conclusions may be affected by bias and systematic errors. Unfortunately, the limitations and the difficulty of access to health units and departments due to the COVID-19 pandemic and the strict measures were obstacles to a more comprehensive and accurate methodological approach. Nevertheless, this effort is a basic indicator of tendencies, which, if it were more accurate, would have provided a steady picture over time, before and during the COVID-19 pandemic. Furthermore, the collected data were based on self-reporting by the participants and no objective measures for smoking verification (such as cotinine levels) were employed.
CONCLUSIONS
Our study showed a significant reduction in HCP smokers during the COVID-19 pandemic, with significantly smaller reduction in smokers among those experiencing high/severe Work-related Burnout versus those experiencing low or moderate Work-related Burnout. Unfortunately, a very significant percentage continues to smoke, and one in three HCP smokers actually smokes more. This is very important, as smoking affects their own health, the health of their patients, and their efficacy in the workplace. Our study also found moderate/low levels of occupational burnout, which are directly correlated with profession (physicians), years of work, and working sector (public sector). Finally, it is noted that HCPs’ smoking habits are inextricably linked with increased Work-related Burnout. It is therefore urgently necessary to reduce smoking prevalence by providing smoking prevention and cessation facilities and programs in HCPs’ workplaces, and by further educating HCPs on smoking cessation strategies and the correct implementation of anti-smoking policies in the workplace. Measures and interventions affecting both HCPs themselves and workplace organization are also necessary in order to achieve a significant reduction of BS among HCPs. The healthcare system should also be reinforced to ensure the effective management of any future crises.