INTRODUCTION
Asthma is a common chronic disease that is estimated to affect as many as 262 million people worldwide, equating to an age-standardized rate of 3416 cases per 100000 population1. In Europe, the prevalence of asthma is calculated at around 8.2% in adults2. A subgroup of these patients with asthma, no more than 5–10%, suffers from severe disease that is partially controlled or uncontrolled despite intensive guideline-based treatment or due to non-adherence to prescribed therapies3. These patients have significantly impaired quality of life (QoL) and account for 40% of all direct costs in asthma4,5. Patients with uncontrolled severe asthma (SA) increase healthcare resource utilization, including a higher number of exacerbations, hospitalizations, and unplanned emergency room visits6 and indirect costs associated with impaired work productivity and absenteeism7.
Epidemiological and patient-centered data on asthma in Greece are somewhat limited. Asthma patients in Greece are mainly managed by pulmonologists and allergists8, and secondarily by general practitioners and internists8,9. Results from a nationwide epidemiological study in a randomly selected sample representative of the adult general population, reported asthma prevalence to be around 6.3%10. Moreover, a population-based, nationwide telephone survey estimated the lifetime self-reported prevalence of asthma at 9.1%11. Data on severe asthma in Greece are even more scarce. In the Greek cohort of the RECOGNISE ‘real-world’ study, most severe asthma patients had poorly controlled asthma, impaired HRQoL, and higher symptom burden12. The total annual costs of asthma from the societal and payer perspective in Greece for 2017 were estimated at €727 million and €547 million, respectively, mostly attributed to patients with not well-controlled asthma13. Patients with SA who remain uncontrolled are eligible for treatment with biological14. According to data from the National Health and Nutrition Examination Survey (NHANES) in the US, about 2.8% of all asthmatics and 85% of those with severe asthma were eligible for at least one biological15. In the Greek cohort of the RECOGNISE ‘real-world’ study, 87% of severe asthma patients were assessed as eligible for biologic treatment by investigator’s judgement12. Although the safety and efficacy of biological treatment in SA have been clearly demonstrated in several randomized controlled trials, qualitative studies exploring patients’ experiences with a patient-reported outcome approach are limited in the literature and basically non-existent regarding the Greek population. This survey aimed to comprehend the patients’ perspectives on living with SA in Greece in terms of symptoms and well-being, and evaluate the impact of biological therapy on patients’ QoL.
METHODS
Study design and participants
A quantitative descriptive survey exploring the experiences of adult patients living with SA was conducted. A total of 221 patients who had a prior confirmed diagnosis of severe asthma were recruited in the study either from 8 different outpatient SA clinics nationwide or an IQVIA panel of patients, between June 2021 and April 2023. The eligibility for severe asthma was based on the requirement for treatment with high-dose inhaled corticosteroids plus a second controller (and/or systemic corticosteroids) to prevent the disease from becoming ‘uncontrolled’ or to remain ‘uncontrolled’ despite this therapy. All patients provided written consent. Patients from the IQVIA panel were recruited through Patient Advocacy Groups or specialized physicians’ practices.
Questionnaire and measures
Data were collected using a specific questionnaire (Supplementary file Section 1). The design of the questionnaire and its attributes were validated through in-depth discussions (interviews and/or focus groups) with SA patients, consisting of 3 mini-focus groups with severe asthma patients with a total sample of 11 participants. The discussion was focused on their everyday concerns/difficulties related to the disease covering the following main topics: unmet needs and ideal treatment for the disease as stated by the patient; journey of the patient from diagnosis to treatment; patient feelings and experience of various treatments (e.g. biologic treatment, ICS/LABA); disease’s impact on patients everyday life-disease burden; perceived quality of life (QoL) as was self-assessed by the patients with the use of a Likert scale from 1 to 5 (1=very poor to 5=very good); relationship with healthcare providers and the healthcare system; source of information for disease; treatments; and new developments. The aim of those in-depth discussions was to provide insights on the questionnaire’s design in terms of the main topics of interest related to patient perspectives of living with severe asthma focusing on patient attitudes and stances towards the disease. Final questionnaires were provided by healthcare professionals in hardcopy or completed online (CAWI: Computer Assisted Web Interviewing). Data were collected and analyzed directly by IQVIA. This survey was conducted in accordance with the Declaration of Helsinki16. This method was used to maximize the use of available data (pairwise deletion). No imputation was used. All participants provided written informed consent prior to survey commencement.
Data analysis
Statistical analysis was performed using SPSS for Windows Release 28.0.1.0. Subgroup means were tested with one-way analysis of variance (ANOVA) for a quantitative dependent variable by a single independent variable, patients on biological treatment or not on biological treatment. Also, a two-proportion Z-test was used to determine whether the two proportions were different from each other. Z-statistics were computed from the two independent samples (i.e. bio-T vs non-bio-T users) and the null hypothesis was that the two proportions were equal. A p<0.05 was considered statistically significant.
RESULTS
Demographics
In total, 221 patients with severe asthma were recruited. Most of them were women and aged ≥45 years17. The detailed demographic characteristics are provided in Table 1.
Perceived QoL of a patient with SA
Severe asthma patients were asked to rate their total QoL, with regard to their disease. Approximately 40.7% of total patients (90/221) expressed a neutral or poor/very poor attitude towards perceived QoL (Table 2). In general, the perceived QoL of patients on biological treatment was significantly higher compared to patients not on biological treatment (Good: 65.2% vs 54.3%, p=0.006) (Table 2).
Impact on patients’ daily life
When patients were asked to rank the importance of a list of abilities in their daily life, completing everyday chores was a priority for both age groups (18–44 years, 90%; and ≥45 years, 94%). The abilities for intense and mild physical activity were statistically the most significant abilities for younger patients (aged 18–44 years) compared to older ones (the ability for intense activity: 72% vs 57%, p=0.0279; and the ability for mild physical activity: 85% vs 72%, p=0.0291, respectively). Also, a statistically significant difference was shown in completing everyday chores without effort between patients on biological treatment and not on biological treatment, with less significance shown in patients not receiving biological treatment (96% vs 88%, p=0.0291).
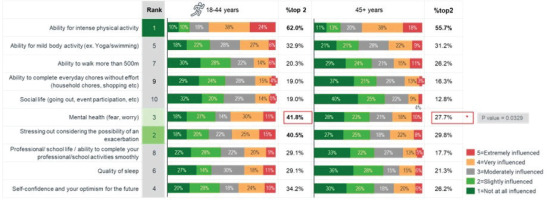
When patients were asked to prioritize the abilities that have been affected the most by their disease, the ability for intense physical activity together with stressing out due to the risk of exacerbation risk and mental health (fear/worry), was ranked on the top of the list (Figure 1). Other abilities that have been ranked on the top of the list of affected abilities were daily chores together with the ability to walk more than 500 m, as well as general optimism for the future (Figure 1).
Figure 1
Degree to which severe asthma has influenced/limited various patient everyday-life abilities among SA patients overall. Abilities influenced by severe asthma in total SA patients. Rated on a scale 1–5, where 1=not influenced at all and 5=influenced very much

SA negatively influenced the physical skills of younger patients, as well as their mental health (41.8% vs 27.7%, p=0.0329) and self-confidence (34.2% vs 26.2%, p>0.005) (Figure 2).
Figure 2
Degree to which severe asthma has influenced/limited various patient everyday-life abilities among SA patients by age. Rated on a scale 1–5, where 1=not influenced at all and 5=influenced very much
Data sub-analysis has shown that a higher percentage of patients on biological treatment compared to patients not on biological treatment seemed to feel more relaxed mentally and less stressed about exacerbations, and thus were more optimistic. The ability for intense physical activity was negatively influenced in all SA patient groups, yet to a lesser degree in patients on biological treatment (48.6% vs 68.6%, p=0.0029) (Figure 3).
Frequency of symptoms
Cough/phlegm were the most frequent symptoms reported by 35% of SA patients followed by 28% talking about dyspnea/shortness of breath (Supplementary file Figure 1a). Patients receiving biological treatment reported significantly lower frequency (ranking 1–2) of symptoms compared to patients not on biological treatment, indicating therapy effectiveness especially in dyspnea and cough (dyspnea/shortness of breath, 62% vs 30%, p<0.0001; cough/phlegm, 63% vs 34%, p<0.0001; chest tightness/chest pain, 76% vs 62%, p=0.0395; night awakenings, 80% vs 64%, p=0.0144; in patients on biologic treatment vs not on biologic treatment) (Supplementary file Figure 1b). Additionally, younger SA patients reported a higher frequency of all symptoms compared to older (aged ≥45 years) patients, especially regarding cough/phlegm (Supplementary file Figure 4).
Fewer patients receiving biological treatment reported frequent symptoms (at least 1) compared to patients not receiving biological treatment (39% vs 53%, p=0.0390) (Supplementary file Figure 1c). More specifically, a higher frequency of all symptoms was reported by patients who were not on biological treatment as well as younger patients (aged <45 years).
Significance of factors associated with asthma control
Overall, most patients (70%) reported high levels of asthma control. The highest rates were met in patients aged ≥45 years compared to younger patients (77% vs 60%, not significant), patients located in Attica compared to the rest of Greece (76% vs 66%, not significant), as well as patients on biological treatment compared to patients not on biological treatment (ranking 4–5: 82% vs 59%, p=0.0002) (Supplementary file Figure 2a).
When SA patients were asked to rank the factors which seemed to affect most treatment satisfaction, reduction of exacerbations (91%) followed by discontinuation of systemic corticosteroids (83%) were the most important considerations for SA patients in assessing satisfaction perspective on their current treatment (Supplementary file Figure 2b). Interestingly, when patients were asked to prioritize the factors in order of significance, better exacerbation control was on average the most significant factor (36%), closely followed by better symptom management (30%).
Group sub-analysis has shown significant differences in factors deemed important for asthma control between patients on biological treatment and not on biological treatment with higher significance given to criteria by patients receiving biologic treatment (exacerbations reduction: 94% vs 88%, p=0.0493; corticosteroids reduction or discontinuation: 90% vs 76%, p=0.0116). On the other hand, patients not receiving biological treatment expressed statistically significantly higher importance on sparse medication as a key factor for the control of their asthma compared to patients on biological treatment (81% vs 68%, p=0.0289) (Supplementary file Figure 2c).
The most anticipated therapeutic benefit of a new treatment for patients receiving biologic treatment was the reduction in SA symptoms/exacerbations (34%) followed by the lower use of drugs/corticosteroids (19%). Statistical significance was shown between treatment groups for reducing symptoms and exacerbations, as potent new treatments benefit. More specifically, better control of symptoms, such as exacerbations, seemed to concern more patients on biological treatment compared to patients not on biologic treatment (34% vs 17%, p=0.0043) (Supplementary Figure 2d).
Severe asthma resources for patients
When patients were asked to prioritize sources of information about their disease, it was found that the attending doctor was the main source of information (89%) followed to a less degree by personal internet research (30%) (Supplementary file Figure 3a). Younger patients together with patients not on biological treatment seemed to be more frequent users of digital sources (43% for patients aged 18–45 years vs 23% for patients aged ≥45 years, p=0.0020; 55% patients on biological treatment vs 27% patients not on biological treatment, p=0.0026).
Moreover, finding an appropriate doctor for SA was not an easy task for a significant percentage of patients (39%) (Supplementary file Figure 3b), especially for patients receiving biological treatment (49.1% vs 26.7%, p=0.0007) and for older patients (aged ≥45 years) (44.7% vs 29.1%, p=0.0232).
Approximately 13% of patients reported a lack of information regarding their condition (Supplementary file Figure 3c). Almost 20% of patients not receiving biological treatment reported a lack of information about SA (18% on biological treatment vs 8% not on biological treatment, p=0.0281). Also, lack of Patient Support Program (PSP) awareness was reported by 48% of patients (Supplementary file Figure 3d), especially among younger patients not receiving biologic treatment and those living in Attica.
Most patients (74%) have never used telemedicine with the lowest rates being observed in patients not receiving biological treatment (78%). When asked if they would be interested in trying telemedicine, less than half of SA patients responded positively. Interestingly, the lowest intention was reported in patients not receiving biological treatment (41%) (Supplementary file Figures 5 and 6).
Awareness of SA clinical trials
Poor awareness of SA clinical trials was reported (Supplementary file Figure 7a), especially among younger patients, patients not receiving biological treatment (not informed: 69% of patients not on biological treatment vs 54% on biologic treatment, p=0.0237), and patients living in Attica. Most of them (85%) had no previous experience with clinical studies (Supplementary file Figure 7b) and the few who did (n=27/221), mainly described a very positive experience.
Moreover, an important proportion of patients (41%) claimed their intention to participate in a SA clinical study (Supplementary file Figure 7c), while a high percentage of don’t know/not available underlines the need for more information delivered to patients about clinical studies to affiliate and have a positive stance with.
DISCUSSION
Our survey aimed to understand the experiences of severe asthma (SA) patients in Greece, focusing on the impact of biologic treatments on their quality of life (QoL) and daily activities. The study found that SA patients experience significant physical and emotional distress due to the risk of future exacerbations, leading to a lower perceived QoL and reduced ability to engage in daily activities. Notably, patients on biological treatments reported higher QoL scores, less influence of SA on their physical and mental health, and a lower frequency of symptoms such as dyspnea and cough. This is the first survey of its kind in Greece, providing valuable insights into the patient experience with SA. Improved education and customized patient support programs will provide patients with resources and knowledge so that they can effectively communicate their needs to all stakeholders involved in their care as well as ensure access to innovative and effective treatments18,19.
Our findings align with similar international studies that link asthma control to factors such as gender, age, and treatment. Patients with uncontrolled asthma in these studies also reported psychological distress and limitations in daily living activities10,20-22. The survey highlighted that younger patients with SA experienced more significant impacts on physical skills and emotional life, corroborating findings that adolescents with asthma are more likely to have anxiety and depression associated with poor asthma control23,24. Differences between patients receiving biological treatments and those not on biological treatment were noted in terms of perceived QoL and symptom frequency, supporting real-world evidence that biologic treatment reduces asthma symptoms and psychological distress25-29. The inclusion of patients’ perspectives in clinical studies is critical to ensure that the outcomes meet the needs of the intervention’s target population30.
Limitations
The survey has several limitations. It primarily represents the perspectives of Greek SA patients and may not reflect national asthma care standards. Data were self-reported by respondents who identified themselves as having asthma, and the SA diagnosis was not independently verified during the interviews. The translation of interviews from Greek may have affected the findings. Additionally, the survey’s scope does not account for all regional variations within Greece, suggesting a need for national epidemiological studies to provide a more comprehensive understanding of asthma management. Such disparities may be attributed to several factors, including environmental risk exposures, poorer access to specialized centers, or differences in socioeconomic status between urban and rural areas31. For example, the sample leans towards older individuals (with 63% of participants being ≥45 years). This age distribution may present potential limitations in accurately representing the general severe asthma population, and consequently the conclusions drawn from this study may not be entirely generalizable to the broader population. Additionally, access to biological therapies for severe asthma can be hindered by multiple factors, including financial barriers, insurance coverage limitations, inadequacies in healthcare systems and policies, and delays in diagnosis and referral to specialist centers32. Furthermore, geographical barriers may present significant challenges in certain contexts, particularly for individuals in rural or underserved regions, who may have limited access to specialist centers that prescribe and manage biologic therapies33. Overcoming these challenges requires a multifaceted approach, including policy modifications, educational initiatives, and improvements to the healthcare infrastructure. Such interventions may be crucial to achieve optimal patient outcomes.
CONCLUSIONS
Severe asthma significantly impacts patients’ QoL, encompassing physical, emotional, and personal aspects. The survey revealed that patients on biological treatment, experience less stress and greater optimism compared to those not on biologic treatment. Despite reporting good control of asthma, many patients still experience frequent symptoms and psychological burdens. The survey also identified a lack of disease awareness and the need for better education and patient support programs. Addressing these unmet needs and incorporating multidisciplinary approaches, including emotional, psychological, and social support, is crucial for improving long-term health outcomes for SA patients in Greece.