The differential diagnosis for diffuse bilateral pulmonary nodules is extensive and includes infections, inflammatory disorders and metastatic malignancy (Table 1)1.
Table 1
Differential diagnosis of diffuse pulmonary bilateral nodules
Minute pulmonary meningothelial-like nodules (MPMN) result from epithelioid cell proliferation within the interstitium, and can present as a solitary pulmonary nodule or, less frequently, as diffuse nodules, termed diffuse pulmonary meningotheliomatosis (DPM)2.
In DPM these cells form small nodules of ground-glass appearance on chest CT scan, with/without central lucency (‘cheerio sign’) throughout the lung tissue and typically present as diffuse and bilateral randomly distributed nodules3. Most are too small to be detected by CT, but the autopsy incidence has been reported as 7.2%4.
DPM/MPMNs are benign and are more common in females with age in the sixth to seventh decade. Patients are often asymptomatic or they may present with non-specific cardiorespiratory symptoms5. The exact etiology remains unclear, however, these nodules are more commonly associated with pulmonary thromboembolic disease or smoking-related interstitial lung disease6. A higher incidence of these nodules has been reported in patients with primary malignant pulmonary tumors, specifically with lung adenocarcinoma4. Definitive diagnosis requires lung biopsy, typically surgical3.
We report a case of diffuse pulmonary meningotheliomatosis in a patient with a past medical history of lung adenocarcinoma.
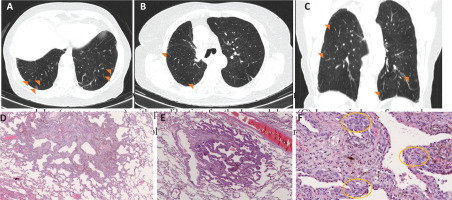
An 81-year-old woman, non-smoker, with a past medical history of stage IA lung adenocarcinoma submitted 3 years before to superior right lobectomy, presented to pulmonary clinic for follow-up and did routine chest CT which showed multiple bilateral micronodules of ground glass appearance, with 2–5 mm, with basal predominance (Figures 1 A, B and C), raising the possibility of metastatic lesions. She denied any symptomatology associated, namely chest pain, dyspnea or systemic symptoms.
Figure1
(A, B) Lung window of axial chest CT scan showing multiple ground glass lung nodules (orange arrows) with predilection for the lower lobes; (C) Lung window of coronal chest CT scan showing multiple ground glass lung nodules (orange arrows); (D, E) Histopathological findings, showing areas of nodular configuration, with expansion of the alveolar septa and architectural preservation; (F) These nodular areas are constituted by polygonal cells, with uniform nucleus (orange circles), with positivity for EMA and vimentin
To study these lesions and evaluate the possibility of a relapse of the malignant disease, she did an 18-FDG PET scan that showed a micronodular pattern in both lungs, functionally uncharacterizable due to the reduced dimensions of the nodules, without any other lesions.
Due to dimensions of the lesions and the difficult approach through CT-guided transthoracic biopsy, a video-assisted thoracoscopic (VATS) biopsy was performed. The histopathological examination revealed that these nodules consisted of pulmonary meningotheliomatosis, excluding metastatic lung lesions (Figures 1 D, E and F). The patient is currently asymptomatic and maintains in follow-up, without signs of malignancy in the 2 years period since the detection of the nodules.
DMP is a relatively rare condition, apparently clinically innocuous and with conservative management3. Despite this, we consider that awareness of this entity is important as it can be confused with other diseases, namely metastatic disease as in the case abovementioned.
Differential diagnosis in these cases can be difficult, especially in patients with history of a concomitant malignancy, and will require correlation with clinical and radiological findings, as well as lung biopsy for definitive diagnosis.