INTRODUCTION
Urinothorax is a rare cause of pleural effusion. The diagnosis usually requires a high index of suspicion and might pose a challenge in cases where the clinical context is not straightforward and/or pleural fluid analysis is not helpful. We present a patient with urinothorax, where the usual diagnostic work-up was unsuccessful and we had to purse alternative imaging tests, such as renal scintigraphy, to solve the problem. We further discuss the existing literature on this topic and try to give possible explanations about the ‘atypical’ presentation of this case.
CASE PRESENTATION
A 75-year-old male, non-smoker, was admitted to the hospital because of dyspnea on exertion that had started a few days previously. The clinical examination and the chest x-ray revealed a right-sided pleural effusion (Figure 1). His past medical history was unremarkable, except for a three years’ history of a right-sided recurrent pleural effusion. The effusion remained undiagnosed until his last hospitalization.
During this three years’ period he had 1–2 admissions per year to the hospital for recurrences of the pleural effusion. In all instances a therapeutic thoracentesis, with complete drainage of the pleural fluid (1.0–1.5 L of serous fluid each time) was performed. The pleural fluid was in all cases exudative with a lymphocyte predominance, negative cytology and cultures, and pH around 7.4. ADA was steadily below 10 IU/L, triglyceride levels <50 mg/dL and glucose >60 mg/dL. In at least three different hospitalizations, creatinine levels in both the pleural fluid and serum were measured and the creatinine pleural fluid/serum ratio was 0.9. Only once was the ratio found marginally increased (1.15). Both routine and immunologic blood tests were normal. At the initial investigation computed tomography (CT) of the chest with pulmonary angiography showed the pleural effusion without other abnormalities. CT of the abdomen was normal, except for a right-sided renal cyst of maximum diameter 7 cm (Figure 2). The patient refused medical thoracoscopy and was left under observation, as an outpatient, since there were long intervals of six or even more months, where he was asymptomatic and without pleural fluid on chest x-ray.
Figure 2
Computed tomography (CT) of the abdomen with intravenous renogram. Contrast enhancement of both kidneys is visible. The asterisk denotes the renal cyst, which caused significant deformation of the right kidney

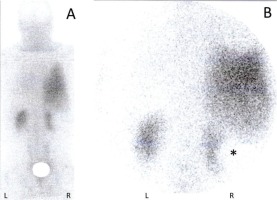
In the last hospitalization, the repetition of thoracentesis, blood tests and CT imaging of the chest and abdomen, did not add any novel diagnostic finding. At this stage, a renal scintigraphy with technetium99m diethylene triamine pentaacetic acid (Tc-99m DTPA) was performed, which revealed accumulation of the radiopharmaceutical at the right hemithorax (Figure 3). The test was diagnostic for urinothorax. An intravenous CT renogram was performed to discover the site of urine extravasation, but it was negative (Figure 2). Neither the renal scintigraphy nor the CT renogram detected a urinoma (the renal cyst itself was ‘negative’ on both examinations, which is compatible with its cystic nature). The patient denied further interventions.
Figure 3
Renal scintigraphy with Tc-99m DTPA. A delayed whole-body scan (A) and a scan of the chest and upper abdomen (B), at 4 hours, demonstrate intense accumulation of the radiopharmaceutical in the right hemithorax. Both kidneys are also visible. The asterisk denotes a photopenic area that changes the shape of the right kidney and corresponds to the large renal cyst (R: right; L: left; Tc-99m DTPA: technetium99m diethylene triamine pentaacetic acid)
DISCUSSION
Urinothorax is the accumulation of urine in the pleural space. It is due to obstructive uropathy or injury to the urinary tract and usually occurs in the hemithorax that is ipsilateral to the underlying uropathy1-3. The mechanism of urine transit to the pleural space is unclear. It seems that urine, after its exit to the retroperitoneal space follows the path of ‘least resistance’ towards the negative pressure of the thoracic cavity, and finally reaches the pleura passing through anatomical defects of the diaphragm. Furthermore, regional lymphatics might have a complementary role in this process2,4,5. In our case, the mechanism of urinothorax was not apparent. However, we believe that the cause was the renal cyst, which lead to the marked distortion of the right renal pelvis. We speculate that, since the patient exercised regularly, physical activity might have been an add-on factor that caused intermittently microtraumas to the distorted pelvis and oozing of urine to the retroperitoneum.
Urinothorax is a rare disease entity. Until the end of 2017, less than 100 cases had been reported3,4. Most publications are case reports of 1–4 patients, so key issues about urinothorax such as clinical course, characteristics of the pleural fluid or management, are not well known. Moreover, the reported information is heterogenic. Some articles highlight the clinical characteristics of the patients while others stress diagnostic and therapeutic aspects. It is not uncommon for the diagnosis to be established without determining biochemical parameters of the pleural fluid such as creatinine pleural fluid/serum ratio, pH, or glucose levels3. In most reported cases, diagnosis was based on the association of a pleural effusion with obstructive or traumatic uropathy, and resolution of the effusion after treatment of the obstruction or trauma1,2.
It is important to note that common perceptions about the pleural fluid characteristics in urinothorax (e.g. odor, its transudative nature, low glucose levels, and pH), are based on a small proportion of the published cases1,3. Toubes et al.3 reviewed the literature until 2017 and found 88 cases with urinothorax. The odor of pleural fluid (urine-like or ammoniacal) was mentioned in only 8 cases. The question of whether it was a transudate was addressed in 32 cases (44% were exudates). Glucose levels and pH were reported in 28 and 26 cases, respectively (6 patients had glucose <60 mg/dL and 16 had pH <7.3). Pleural fluid/serum creatinine ratio was calculated in 48 of the 88 patients and, in all but one, it was found >1.
These observations imply that apart from the heterogeneity of the reported information, pleural fluid characteristics in urinothorax present a high degree of variability, which means that pleural fluid might not always resemble urine3,4,6. The reasons for this variability are unknown. It has been postulated that trauma or hemorrhage at the site of urine extravasation may change the constituents of urine3. In the retroperitoneal space, an interchange of soluble substances between urine and surrounding tissues cannot be excluded. Moreover, the composition and biochemical makeup of urine might change over time in the pleural cavity6,7. Comorbidities (such as congestive heart failure or infection) may also alter the chemistry of ‘pleural urine’4. Consequently, the different clinical context, in each individual case, might account for the diversity of pleural fluid characteristics in urinothorax.
In the presented case, the absence of ‘typical’ features of urinothorax in the pleural fluid, and especially the repeatedly low pleural/serum creatinine ratio, delayed the diagnosis for about three years. Only renal scintigraphy, finally, revealed the source of pleural fluid. Tc-99m DTPA is lipid insoluble and therefore does not enter the cell. It is almost entirely removed from circulation by glomerular filtration8,9. These properties (i.e. stability and complete elimination by the kidneys) make renal scintigraphy with this radiopharmaceutical an excellent confirmatory test for urinothorax, because the only way for Tc-99m DTPA to reach the pleural space is via translocation of urine into the pleural space4,6.
A pleural fluid/serum creatinine ratio >1 has frequently been considered a hallmark of urinothorax2-4. However, it should be interpreted cautiously in conjunction with the other clinical and laboratory findings. Values >1 may be found in pleural effusions of different origin1. On the other hand, values <1, although they seem to be exceptional in urinothorax, should not dissuade clinicians from this diagnosis3,7.
CONCLUSION
The diagnosis of urinothorax demands a high index of clinical suspicion. Reliance on pleural fluid biochemical indices alone, to exclude or confirm urinothorax, might be misleading. In doubtful cases it is prudent to pursue more accurate tests, such as renal scintigraphy with Tc-99m DTPA, to solve the clinical problem.