INTRODUCTION
Tracheal diverticula (TDs) are benign conditions that belong to the larger group of paratracheal air cystic (PTAC) lesions1. Incidence is around 2.4%2. It is an outpouching of the tracheal wall and usually projects to the right side of thoracic inlet due to the presence of esophagus on the left. It can be congenital or acquired; single or multiple3. It is usually asymptomatic and is thus underdiagnosed. However, it has the potential to act as a reservoir of sputum thereby leading to recurrent upper respiratory tract infections or can lead to other symptoms such as chronic cough, hemoptysis, dysphagia, stridor or dyspnea4. Tracheal diverticulum can also be associated with abnormal pulmonary function and obstructive lung disease mainly emphysema5. Obstructive diseases or chronic cough can lead to long standing increased intraluminal pressure which can then lead to development of diverticulum in the areas of diminished resistance of the tracheal cartilage1. Usually, asymptomatic cases are managed conservatively when diagnosed but surgical or conservative treatment might be required for symptomatic patients, depending on patient age and physical condition. We present two asthmatic cases who had chronic cough and were later found to have tracheal diverticulum.
CASE PRESENTATION
Case 1
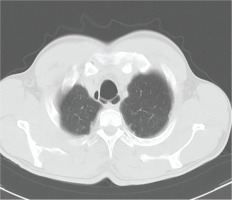
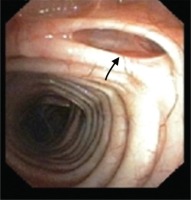
A 39-year-old asthmatic male, working in a wheat flour mill with no comorbidities presented with complaints of cough with expectoration and shortness of breath for last 10 years (increased since last 15 days). He had repeated exacerbations and respiratory tract infections in spite of asthma being well controlled on treatment (LABA+ ICS) in the past without any other significant past history. On auscultation, the patient had bilateral wheeze during expiration with crepitations in both infra-scapular and infra-axillary areas. CXR showed bilateral bronchiectasis. CT scan showed bilateral tractional and cystic bronchiectasis, AP diameter of trachea was around 2.9 cm and a few paratracheal cysts were seen with one communicating with the trachea. A tracheal diverticulum with extroflexion of mucosa and no cartilaginous defect was also seen (Figure 1). For further evaluation, bronchoscopy was done that showed flaccidity of tracheal wall with marked enlargement of trachea with tracheobronchial diverticulosis. Narrowing of left lower bronchus opening with bronchial diverticula, full of mucoid secretions was seen (Figures 2 and 3). Thus, tracheal diverticulum was possibly the cause of chronic cough and repeated infections in this patient. As cough was the only symptom, he was managed conservatively with antibiotics, antitussives, expectorant and LABA+ ICS and was advised chest physiotherapy to prevent collection of sputum and repeated infections. He responded well to the treatment and is on regular follow-up.
Case 2
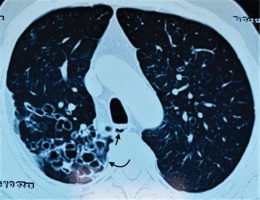
A 50-year-old asthmatic male on treatment for the last 25 years presented with acute exacerbation in the emergency department. In spite of being compliant with LABA+ ICS, he had a repeated history of exacerbations in the past. On chest auscultation, the patient had bilateral rhonchi in all areas. CXR showed bilateral hyperinflated lungs with homogenous opacity in the right upper zone. Sputum AFB and CBNAAT were negative. CECT chest showed central, cystic and varicoid bronchiectatic changes with peri-bronchial thickening in bilateral lung parenchyma more in right upper lobe. It also showed two tracheal diverticula measuring 7×3.6 mm and 9×8 mm along the right posterolateral wall of trachea (Figure 4). Total IgE and Aspergillus specific IgE were within normal limits (337 and 0.08 IU/mL, respectively). The patient did not give consent for Fiberoptic Bronchoscopy. The patient was managed symptomatically for asthma exacerbation with inhaled corticosteroids, bronchodilators and chest physiotherapy, and kept on regular follow-up for prevention of infection and further exacerbations. On regular follow-up the patient is stable.
DISCUSSION
Paratracheal air collections (PTACs) are usually found as incidental findings. They include tracheal diverticulum, laryngocele, pharyngocele, Zenker’s diverticulum, apical hernia of the lung, and apical bullae6. Tracheal diverticulum consists of small air collections at the paratracheal area lined by ciliated columnar epithelium2. It is a rare benign disease which is usually asymptomatic. If symptomatic, symptoms may be due to either collection of sputum leading to superadded infections or to the compression of adjacent organs. It can be congenital or acquired. Congenital tracheal diverticulum occurs mainly due to defects in tracheal cartilage during fetal development and contains all the layers of tracheal wall7. Acquired tracheal diverticulum can occur either due to the long standing increased intraluminal pressure caused by chronic cough or due to a weakened tracheal wall as a result of repeated respiratory infections8. According to the literature the most common cause of acquired tracheal diverticulum is chronic cough6 and it may arise at any level. Acquired tracheal diverticulum is typically wide-mouthed and larger in size than congenital TD2.
CONCLUSION
The occurrence of tracheal diverticulum has been rarely reported in asthmatic patients in the English literature, and whether the diverticulum is congenital or acquired in these patients is unknown. There is insufficient evidence to recommend the optimal therapeutic schedule at present. Asymptomatic TDs usually do not require any treatment. Symptomatic TDs may require conservative treatment such as anti-inflammatory, postural drainage, and antibiotics. However, if there is compression of adjacent organs, recurrent infections or severe symptoms then transcervical resection or endoscopic laser surgery or electrosurgery can be considered7. Our case patients were managed conservatively and are stable on regular follow-up. It needs to be emphasized that TDs should also be considered as a cause of chronic cough and high degree of suspicion should be there, as they may lead to serious complications.