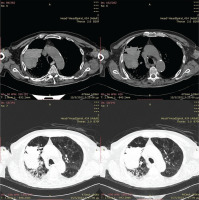
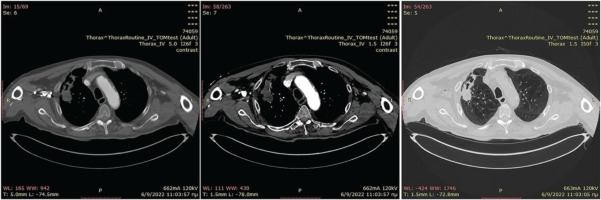
Thorax Magnetic Resonance Imaging (MRI) is not routinely used in clinical practice for characterization of lung lesions, as presence of air in the lungs results in considerable reduction of the MRI diagnostic accuracy. We present a case of a 69-year-old patient, bedridden for the past year due to hemorrhagic stroke, who was transferred to the Emergency Department, due to breathlessness and productive cough. Microbiological exams revealed anemia (Hb: 9.9 g/dL), moderately elevated C-Reactive Protein (CRP) value (4.33 mg/dL, with normal values <0.5 mg/dL) and procalcitonin (PCT) value within normal range (0.03 ng/mL, with normal values <0.05 ng/mL). Blood and urine cultures were negative. The patient had a smoking history of 35 pack-years. CT imaging revealed a large lesion of the right upper lobe (Figure 1). The patient underwent CT guided FNA of the lesion twice, without findings suggestive of a definite diagnosis. A chest MRI was then conducted (Figure 2), revealing diffusion restriction in the diffusion-weighted imaging (DWI) of the upper right lobe lesion. Empiric treatment with amoxicillin-clavulanic acid 1 g × 3 was initiated, resulting in gradual increase of body weight and diminution of the lesion in the chest CT imaging on 3 months of treatment (Figure 3).
Figure 2
a) Thorax MRI, T1 vibe Fat-Sat contrast. Tumor-like lesion of the right upper lobe with ring like enhancement and necrosis. b) Diffusion weighted image (DWI), intense diffusion restriction in the cystic part of the lesion. c) ADC map 500 mm2/sec
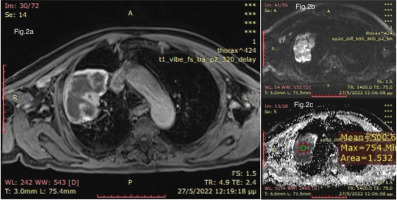
Figure 3
Chest CT on 3 months of antibiotic treatment with marked decrease of the right upper lobe lesion
One of the main utilities of diffusion-weighted MRI sequences is the differentiation of abscess from malignant mimicker (tumors with central necrosis) and thus they are broadly used in combination with ADC map, in brain and liver MRI1-3. Despite that both malignancy and abscess can restrict diffusion in diffusion-weighted MRI sequences, there are some distinct differences in the restriction pattern between them which can lead to the differential diagnosis1,2. Abscesses manifest intense restricted diffusion in their cystic necrotic compartment, with high DWI signal and particularly low signal in ADC maps (usually <800 mm2/s). Tumors may manifest diffusion restriction only in their enhanced solid compartments. On the other hand, the cystic-necrotic compartment of the tumors shows no restricted diffusion with low DWI signal and high ADC signal.
In our case using the DWI techniques, we found diffusion restriction in the cystic-necrotic lesion with a very low ADC map value, strongly suggesting the presence of an abscess. Opposed to Fluorine 18-FDG PET/CT, diffusion-weighted MRI was not suggested by the 2017 Fleischner Society guidelines for the management of incidental pulmonary nodules4. However, findings from a recent meta-analysis of the limited studies comparing Fluorine 18-FDG PET/CT to diffusion-weighted MRI for the differential diagnosis of malignant versus benign pulmonary lesions, support the equally high diagnostic accuracy of diffusion-weighted MRI for a lower cost and less radiation exposure5. Consequently, a 2022 Fleischner Society position article suggests the use of diffusion-weighted MRI in clinical practice for lung nodule characterization and highlights that there is promising data for its use in cases of pulmonary parenchymal abnormalities1.