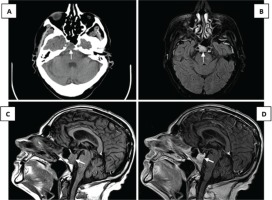
A 68-year-old man with a recent diagnosis of small cell lung carcinoma, presented for a routine evaluation at our local lung cancer department, aiming to start treatment with carboplatin and etoposide. During the evaluation he seemed disoriented and complained of a headache. On physical examination only spatiotemporal disorientation stood out on the neurologic examination, with no other changes to report. Blood tests revealed hyponatremia, and elevated creatinine, alkaline phosphatase, gamma-GT, bilirubin, C reactive protein and procalcitonin. He was then admitted and treated for possible urinary infection, later confirmed by positive urine and blood cultures for Escherichia coli. Considering maintained symptoms, he was further investigated with a head CT scan with contrast to rule out brain metastases and it end up revealing a sphenoidal osteolytic lesion measuring 20×20×14 mm (Figure 1A), in addition to other smaller cranial bone metastases. Head MRI was also requested to allow a better characterization, showing an osteolytic lesion centered on the right paramedian region of the basisphenoid, with pronounced hyperintensity on T2-FLAIR images (Figure 1B), and homogeneous signal enhancement after contrast administration (Figures 1C and 1D).
Figure 1
Head CT (A), axial plane: sphenoidal osteolytic lesion measuring 20×20×14 mm. Head MRI, axial T2 FLAIR-weighted images (B): osteolytic lesion centered on the right paramedian region of the basisphenoid, with pronounced hyperintensity. Head MRI, T1-weighted sagittal images, before (C) and after (D) gadolinium contrast administration: homogeneous enhancement of the lesion
The case presented poses an unusual finding. Although imaging study was performed to clarify the presence of brain metastases, the sphenoid metastasis was not expected, and it was found by chance. Patients with lung cancer are at a higher risk of developing bone metastases (around 40%), but sphenoid bone metastasis is rarely seen1-3.
Symptoms resulting from metastatic compression and compression of cranial nerves (such as ocular symptoms, headache, and facial dysesthesia) may occur and the physician should always be aware of them2,4.
The patient eventually passed away after a second cycle of chemotherapy, due to deterioration of the general condition, with worsening of renal function, anemia and grade I mucositis.


