Pulmonary sequestration (PS) is a rare congenital malformation with an incidence of 0.1%, representing 0.15–6.4% of all pulmonary malformations, with only 10% manifesting in adulthood1,2. It is characterized by a non-functioning pulmonary parenchyma vascularized by an aberrant artery branch from the systemic circulation1. These are classified into intralobar and extralobar, with intralobar being the most frequent. Concomitant congenital anomalies are associated with extralobar PS in 43% of cases, however in intralobar PS are only seen in 17%3. The combination of pulmonary sequestration with pectus excavatum is described in children, although the presentation in adulthood is rare. We present a case of intralobar PS that occurred in adulthood with concomitant pectus excavatum.
A 39-year-old female non-smoker with past medical history of pectus excavatum was presented to the pulmonology outpatient department with dry cough and left pleuritic chest pain. Respiratory examination showed decreased breath sounds in the lower left hemithorax. Chest radiograph exposed a homogeneous opacity in the lower third of the left hemithorax. Chest Computed Tomography (CT) scan was performed and revealed a small collapse of the left lower lung associated with small pleural effusion. CT scan also determined the pectus severity index (PSI) as 2.9. Due to a suspicion of left pleural effusion, ultrasound-guided thoracentesis was scheduled. However, chest ultrasound excluded the presence of pleural effusion, exposing parenchymal consolidation and thoracentesis ended up not being performed. CT scan was repeated, this time with intravenous contrast, and showed an anomalous vessel originating from the distal thoracic aorta irrigating posterior and medial segment of left lower lobe, compatible with intralobar PS (Figures 1 A, B and C). Pulmonary function tests showed no significant ventilatory changes. Transthoracic echocardiogram was performed and showed a good global systolic function, without changes in segmental contractility or valvular abnormalities. The patient was referred to the thoracic surgery and was proposed Video-Assisted Thoracoscopic (VATS) left lower lobectomy with anomalous vessel lacquering (Figures 1 D and E). Although she had PSI lower than 3.25 and no cardiorespiratory function alteration or concerns about appearance, the possibility of pectus excavatum surgical correction was suggested, which the patient refused. The procedure was uneventful and the patient was discharged on 8th post-operative day; currently being under surveillance with resolution of symptoms.
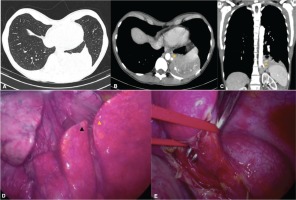
Figure 1
CT scan with contrast revealed a homogeneous mass (A) and the presence of aberrant arterial branch of the distal thoracic aorta (arrow) irrigating posterior and medial segment of left lower lobe (B, C). VATS photo showed a pulmonary consolidation of medial and posterior segment of left lower lobe (black arrow and yellow arrow, respectively, D) and aberrant arterial branch of the distal thoracic aorta (E)
A total of 12 cases of PS associated with pectus excavatum were identified in English literature, all in pediatric age, 11 of those associated with intralobar subtype2-5. The causes of pectus excavatum include connective tissue disorders and neuromuscular diseases. In addition, it can also occur in response to an underlying lung condition4. The etiology is not clear, there are currently several hypotheses. However, considering that it is only associated with intralobar PS, Iva and Watanabe4 suggest that the combination of anatomical and physiological factors, such as changes in ventilatory mechanics caused by sequestration, contribute to thoracic deformation both in embryogenic development and after birth.


