INTRODUCTION
Chest trauma injuries are one of the main causes of death in young people and include lung contusions, lacerations, pneumothorax, hemothorax, rib fractures and tracheobronchial injuries1,2. Pulmonary contusion is the most common identified entity after trauma and usually results from blunt chest trauma (traffic accidents, falls from great heights), shock waves associated with penetrating chest injury, or explosion injuries3,4. Unlike contusion, pulmonary laceration results in disruption of the architecture of the lung and could potentially cause more serious damage. Pulmonary lacerations are commonly caused by penetrating trauma and result in formation of one or multiple cavities filled with air, blood, or both5. In this report, we present a case of lung contusion and laceration in a 19-year-old patient after a motorcycle accident.
CASE PRESENTATION
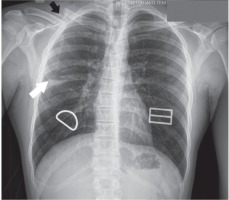
A 19-year-old patient, non-smoker, without previous medical history, presented to the emergency room due to fever and pain at the right periorbital area of the face after a motorcycle collision twenty-four hours ago. The patient was examined initially by general surgeons. He was febrile (38℃) and hemodynamically stable. His oxygen saturation was normal (SatO2: 98% breathing room air) and he had normal breath sounds in auscultation. From physical examination, he presented with bruise injuries in the right side of the face and a right periorbital hematoma. His laboratory examinations revealed normal hemoglobin (15.9 g/dL), elevated white blood cell count (14.90 K/μL with 78.7% neutrophils), elevated creatine kinase (956 U/L) and elevated C reactive protein (96.9 mg/L). After exclusion of SARS-Cov-2 infection, he underwent computed tomography (CT) of the head which showed fracture displacement of the right maxillary sinus and orbitally wall, air-fluid level within injured sinus and right periorbital hematoma (Figure 1). The patient was admitted to the Oral and Maxillofacial Surgery Department for further management with reconstructive surgery. Upon admission, a chest X-ray revealed a cavitary lesion in the right middle lung zone and a fracture displacement of the right clavicle (Figure 2). Chest CT confirmed a fracture displacement of the right clavicle without pneumothorax as well as three cavitary lesions with air-fluid level within the minor and major fissure of the right lung with maximum diameter of about 3.7 cm and adjacent ground glass opacities (Figure 3). Pulmonary preoperative evaluation was performed and the working diagnosis of pulmonary laceration with contusion post-acute chest trauma was made. Thorough evaluation for common and specific pathogens for lower respiratory tract infection proved insignificant. The patient received empirical antimicrobial treatment with ampicillin/sulbactam and azithromycin for superinfection, oxygen therapy with high fractions of inspired oxygen to increase the resolution rate of the cystic lesions and was systematically monitored. Multidisciplinary discussion between pulmonologists, the treating surgeons, the anesthesiologists and the thoracic surgeons led to the decision to postpone imminent surgical management in order to minimize the risk of pneumothorax under positive pressure due to generalized anesthesia. Surgical reconstructive management was undertaken two weeks later without any complications after a new chest X-ray and CT revealed remission of the laceration and contusion lesions (Figures 4 and 5). The patient was discharged from hospital in a very good condition.
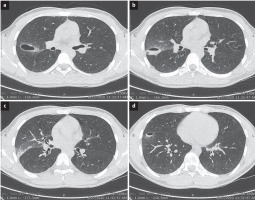
Figure 1
CT of the head which revealed fracture displacement of the right maxillary sinus and orbitally wall (white arrow), air-fluid level within injured sinus (black arrow) and right periorbital hematoma (arrow head)
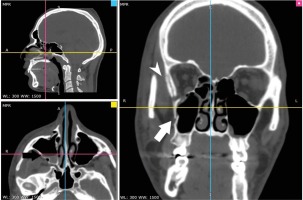
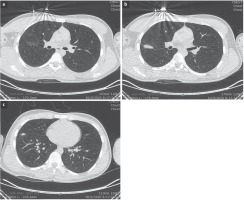
Figure 2
Chest X-ray on admission showing a cavitary lesion in the right middle lung zone (white arrow) and a fracture displacement of the right clavicle (black arrow)
DISCUSSION
A pulmonary contusion is an injury to the lung parenchyma which usually occurs from blunt chest trauma and results in alveolar hemorrhage. As a pathology, it was first described in 1761 by an Italian anatomist, Morgagni6, while the term pulmonary contusion was coined in the 19th century by Dupuytren, a French military surgeon7. Widespread use of explosives during the time of World War I and II led to increased recognition of contusion due to blast injuries4. The most common causes are traffic accidents, pedestrian injuries, falls from great heights, explosions and sports injuries3. The mechanism is the disruption of alveoli and capillaries due to rapid compression and decompression of the chest wall. Alveolar hemorrhage and few hours later interstitial oedema develop in the afflicted parenchyma6,8.
Patients can present with symptoms ranging from minimal to severe, including cough, chest pain, hemoptysis, dyspnea, tachypnea, and hypoxemia. Breath sounds may be decreased, while hematoma and subcutaneous emphysema may be present9. In chest X-rays, findings may not be apparent until 48 hours post-injury10, while chest CT is a more sensitive imaging technique11. Studies have also shown that chest ultrasonography could be useful for the diagnosis of contusion12,13. Ground glass opacities may be present in mild cases whereas widespread consolidations may indicate severe injury14. Specific treatment is often not required and supportive care with prevention of respiratory failure, pain control, management of airway drainage and adequate intravenous fluid replacement are the primary aims of therapy4. In severe cases with development of acute respiratory distress syndrome (ARDS) non-invasive positive pressure ventilation or invasive ventilation may be used3. Surgical stabilization may be required in the case of multiple rib fracture/flail chest3. Contusions usually resolve with supportive care in 5–7 days3, while findings in X-rays may disappear after 10 days8. Pulmonary lacerations are often associated with pulmonary contusions15. They are usually caused by penetrating chest trauma but can be seen after blunt trauma as well16,17. They were first described in 1940 by Fallon18. The mechanism is rupture to alveoli due to compressive forces applied to the lung parenchyma and the concomitant retraction of the surrounding elastic tissue resulting in the formation of small cavities that are filled with air or blood19. These entities are mostly observed in patients aged <30 years, due to the greater compliance of the thoracic cage20. The diagnosis of pulmonary laceration often requires a high index a suspicion. Clinical symptoms are usually non-specific and consist of chest pain, cough and hemoptysis21. Chest CT evaluates more accurately these lesions in comparison to chest X-rays16. Pulmonary laceration can be seen as single or multiple cavities, unilateral or bilateral, commonly seen in the lower lobes, resolving within weeks16. No specific therapy is required unless complications such as superinfection, abscess formation, rupture into the pleural cavity with development of pneumothorax or hemorrhage occur. If patients with pulmonary lacerations need to undergo any surgical procedure under general anesthesia, there is a greater risk of developing pneumothorax under positive pressure ventilation and thoracic surgeons or other trained personnel should be available to manage such complications22.
CONCLUSION
Chest trauma injuries are one of the main causes of death in young people and include lung contusions, lacerations, pneumothorax, hemothorax, rib fractures and tracheobronchial injuries. Patients present symptoms ranging from minimal to severe, including cough, chest pain, hemoptysis, dyspnea, tachypnea, and hypoxemia. Findings may not be apparent immediately after injury and chest CT is the most sensitive imaging technique for diagnosis.