INTRODUCTION
Adenoid cystic carcinomas (ACC) are rarely encountered tumors with a propensity for frequent recurrences originating from secretory glands of the tracheobronchial system that comprise 0.04–0.2% of all lung cancers. Previously classified as benign tumoral lesions, they are currently grouped under low-grade malignant tumors1.
Although uncommonly encountered, they can lead to life threatening central airway obstruction (CAO). They progress insidiously, slowly growing longitudinally within the airways. Frequently patients are incorrectly diagnosed with and treated for asthma or chronic obstructive pulmonary disease (COPD). In patients who have already been diagnosed with ACC, worsening respiratory symptoms can be erroneously attributed to comorbidities or side effects of oncologic treatments. Consequently, both the initial diagnosis and the detection of disease progression can be delayed1,2.
The treatment of choice is surgical resection. The longterm prognosis is favorable if surgery results in complete removal. Postoperative radiotherapy or/and chemotherapy is needed if residual tumor is found at the resection margin. Despite these treatments, rates of recurrence and local invasion remain high1,3. IBP is considered in patients who are not candidates for surgery or having tumor recurrence and when emergency treatment of airway obstruction is required. Securing the airway by IBP offers quick symptomatic palliation and can sometimes allow patients more time until surgery. Some studies have reported that IBP can have long-lasting effects and a success rate comparable to surgery4,5.
ACC requires long-term follow-up because of its slowly progressive nature, high recurrence rate and the younger age of cases compared to other pulmonary malignancies. The management of ACC remains challenging because of the paucity of information on this subject, particularly in interventional pulmonology (IP) unit1,6.
We therefore reviewed the preferred treatment modalities, their success and complications in cases with ACC that underwent IBP in our IP unit, in the light of available literature.
METHODS
Study design and population
We retrospectively examined the demographic data, presenting symptoms, bronchoscopic findings, diagnostic procedures, treatment modalities and outcomes of patients with a diagnosis of ACC who underwent IBP in our IP unit at the Yedikule Chest Diseases and Thoracic Surgery Training and Research Hospital, University of Health Sciences, Turkey, between January 2009 and December 2020, by reviewing patient files and computerized patient records. The procedures were performed after obtaining written and verbal consent from patients according to the Helsinki Declaration and our institutional consent practices. Our study was approved by the ethics committee of University of Health Sciences Turkey, Yedikule Chest Diseases and Thoracic Surgery Training and Research Hospital (Reference number 2020-60, date 17.12.2020).
Flexible bronchoscopy
Flexible bronchoscopy was performed in our bronchoscopy unit under conscious sedation with intravenous midazolam 0.05–0.10 mg/kg and topical lidocaine (maximum dose: 8 mg/kg) with fiberoptic bronchoscopes (Olympus Medical Co., Tokyo, Japan/ Pentax Medical Co., Tokyo, Japan/Fuji Photo Film Co., Japan) for surveillance bronchoscopies and through the rigid bronchoscope to reach distal airways.
Rigid bronchoscopy
Procedures were performed under general anesthesia. All patients were monitored with electrocardiography and for SpO2 during the procedure, with arterial blood pressure measured every 5 minutes. General anesthesia induction was achieved with midazolam 0.05–0.10 mg/kg, propofol (maximum dose: 1000 mg), remifentanil (maximum dose: 2 mg), and rocuronium (maximum dose: 50 mg), with the dosage adjusted to the patient’s condition. The equipment used in the procedures included the Dumon Series II rigid bronchoscopes (Efer Endoscopy, La Ciotat, France) with optical system. Argon plasma coagulation (APC) (40 W, blended mode/continuous flow) was applied using an instrument by ERBE Elektromedizin GmbH, (Tubigen, Germany). Endoluminal treatment was accomplished with a diode laser operating at a wavelength of 980 nm with 4–25 W in pulsed mode (Biolitec Cerals D25; Germany). Cryo-therapy was performed with the ERBOKRYO system (Elektromedizin GmbH, Tubingen, Germany).
Airway obstruction was defined as >50% obstruction of the tracheobronchial lumen within the reach of a rigid bronchoscope. The degree of obstruction was determined based on the Cotton-Myer grading for tracheal stenosis. Success of treatment was defined as >50% relief of the obstruction and reconnection with the distal airway, accompanied by clinical improvement.
Findings detected bronchoscopically in the tracheobronchial system were grouped as external compression, mucosal/submucosal infiltration, and endoluminal mass.
Acute complications related to interventional bronchoscopic procedures were defined as ‘complications seen during the procedure and post-procedural first 24 hours’ such as inability to wean from mechanical ventilation, bleeding, arrhythmia, etc.
Statistical analysis
Statistical analysis was performed using the SPSS 16 software (SPSS, Inc., Chicago, IL, USA). All categorical variables are presented as frequencies and percentages. Variables are given as mean with standard deviation, continuous variables are presented as median and range. Survival time was defined as the interval between the diagnosis date for post-surgery/oncologic treatment patients or first-line IBP at the time of diagnosis and mortality due to lung cancer or the date of the last follow up.
RESULTS
Demographic and clinical characteristics
Among 671 patients who underwent IBP for malignant airway obstruction in our IP unit, 13 (1.9%) had a diagnosis of ACC. Their mean age was 54.61±8.7 years and 9 (69.2%) were male. Two (15.4%) were current smokers, 5 (38.4%) were former smokers and 6 (46.2%) were never smokers. Presenting symptoms included dyspnea (76.9%) and hemoptysis (23%). Seven (53.8%) patients with findings of stridor and wheezing on physical examination had been treated with bronchodilators for presumed asthma and COPD. Six (46.2%) patients had extrapulmonary comorbidities (Table 1).
Table 1
Characteristics of study population
| Characteristics | n (%) |
|---|---|
| Male | 9 (69.2) |
| Smoking status | |
| Active smoker | 2 (15.4) |
| Ex-smoker | 5 (38.4) |
| Never smoker | 6 (46.2) |
| Patients with comorbidities | |
| Pulmonarya | 7 (53.8) |
| Extrapulmonaryb | 6 (46.2) |
| Symptoms | |
| Dyspnea | 10 (76.9) |
| Hemoptysis | 3 (23.0) |
| Cough | 1 (7.6) |
| Presentation mode | |
| Post-surgery/oncologic treatment | 5 (38.5) |
| First diagnosis | 8 (61.5) |
| Thoracic computerized tomography available | 11 (84.6) |
| Tracheobronchial (central airway) lesion | 10 (90.9) |
| Tracheobronchial (central airway) lesion + parenchymal invasion | 1 (9.1) |
Thoracic CT images were available for review in 11 patients. Ten patients (90.9%) had only endotracheal and/ or endobronchial involvement, while 1 patient had additional parenchymal involvement (Table 1).
Bronchoscopic findings and management
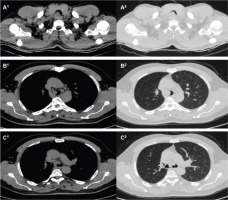
Five patients (38.4%) previously treated with surgical resection had been referred to our center by thoracic surgery and oncology clinics due to suspected recurrence. Eight patients were diagnosed with ACC at our center. Ten patients (76.9%) had tracheal, 5 (38.4%) right main bronchial, and 5 (30.7%) left main bronchial involvement. This involvement manifested as endoluminal mass in 11 patients (84.6%), as mucosal infiltration in 5 (38.4%) and external compression in 2 patients (15.3%) (Figure 1, Table 1). The mean percentage of obstruction due to ACC was 77±13.9% at the trachea, 86±16.7% at the right main bronchus and 65±10.0% at the left main bronchus.
Figure 1
Thoracic computerized tomography sections showing tracheobronchial involvement due to adenoid cystic carcinoma (ACC). A: Soft tissue density due to ACC obstructing the lumen of proximal trachea. B: Soft tissue density due to ACC obstructing the lumen of distal trachea. C: Soft tissue density due to ACC obstructing both right and left main bronchus lumens
Patients had undergone a total of 77 procedures, including 44 rigid bronchoscopies (RB), 31 flexible bronchoscopies (FB) and 2 endobronchial ultrasonographies (EBUS).
The median number of procedures per patient was 1 (range: 1–34), median number of RB was 1 (range: 1–15). Eight patients had not undergone FB. The median number of FBs in the remaining 5 patients was 1 (range: 1–19). Seven patients had undergone only 1 IBP, while 6 (46.2%) had undergone multiple IBPs. The median number of procedures in these patients was 7 (range: 2–34).
Therapeutic procedures performed during IBPs included, in order of frequency, argon plasma coagulation (APC) 31 (38.9%), cryo 19 (24.6%), stenting 4 (5.1%), laser 3 (5%) and cauterization 1 (1%). These procedures were selected and performed in combination according to lesion characteristics (Figure 2, Table 2).
Table 2
Bronchoscopic findings of adenoid cystic carcinoma, treatment modalities used, complications and mortality
| Variables | n (%) |
|---|---|
| Procedures | 77 (100) |
| RB | 44 (57.1) |
| FB | 31 (40.2) |
| EBUS | 2 (2.5) |
| Number of patients with single/ multiple procedures | |
| 1 | 7 (53.8) |
| >1 | 6 (46.2) |
| Number of procedures per patient, median (range) | |
| FB | 1 (1–15) |
| RB | 1 (1–19) |
| Tumor location | |
| Trachea | 6 (46.1) |
| Right main bronchus | 2 (15.3) |
| Left main bronchus | 1 (7.6) |
| Trachea + Right main bronchus | 1 (7.6) |
| Trachea + Left main bronchus | 1 (7.6) |
| Trachea + Right man bronchus + Left main bronchus | 2 (15.3) |
| Types of lesions | |
| Endoluminal lesion | 10 (76.9) |
| Mucosal infiltration | 5 (23.0) |
| External compression | 4 (7.6) |
| Mixed type lesion | 6 (46.1) |
| Location (n) and percentage (mean±SD) of airway obstruction | |
| Trachea | 10 (77±13.9) |
| Right main bronchus | 5 (86±16.7) |
| Left main bronchus | 4 (65±10.0) |
| Interventional bronchoscopic treatment modality | |
| Argon plasma coagulation | 31 (40.3) |
| Mechanical resection | 30 (38.9) |
| Cryo | 19 (24.6) |
| Stenting | 4 (5.1) |
| Laser | 3 (3.8) |
| Cautery | 1 (1.2) |
| Complications | |
| Acutea | 3 (6.8) |
| Chronicb | 0 (0.0) |
| Procedure-related complications | 17 (38.6) |
| Stent-related complications | |
| Granulation | 8 (18.2) |
| Mucostasis | 7 (15.9) |
| Migration | 1 (2.3) |
| Biofilm | 1 (2.3) |
| Number of patients underwent IBPs for tumor recurrence | 6 (30.7) |
| Following surgery/oncologic treatment | 4 (80.0) |
| First diagnosis | 2 (25.0) |
| Survival status of patients | |
| Alive | 9 (69.2) |
| Deceased | 4 (30.8) |
| Mean age of patients (years±SD) | 54.6±8.7 |
| Alive | 52.8±4.8 |
| Deceased | 58.5±14.7 |
| Folllow-up duration (months), median (range) | 38.9 (7–112) |
| Alive | 47.6 (7–112) |
| Deceased | 15.5 (4–44) |
| Folllow-up duration (months), median (range) | 38.9 (7–112) |
| Patients with stent | 67.3 (38–112) |
| Patients without stent | 26.3 (4–66) |
Figure 2
Bronchoscopic appearance of adenoid cystic carcinoma (ACC), before and after the interventional bronchoscopic procedures (IBPs). A1: The right and left main bronchi were obliterated because of the external compression of trachea by ACC. A2: A Silicone Y-shaped stent was inserted after IBP to secure airway patency. B1: Tumoral lesion with endoluminal component extending from the distal end of the trachea to carina. B2: Airway patency was established after IBP. C1: Mucosal tumoral infiltration at mid-trachea. C2: Airway patency established after IBP
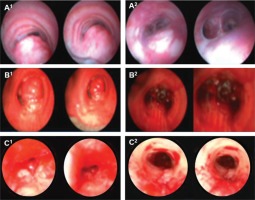
Airway patency was established and dyspnea improved markedly following the first-line IBP in 93% of the cases. The airway patency of all patients except 3 (23%) has been maintained throughout the follow-up period.
The rate of early complications developing in the first 24 hours was 6.8%. One patient had required intensive care treatment on two separate occasions due to development of moderate haemorrhage and respiratory acidosis, while a second patient developed pneumothorax needing tube thoracostomy. No mortality resulted from early complications. Late complications were seen in 33.7% and were all stent related. Among 4 patients who were stented, 3 (75%) developed mucostasis, 3 (75%) granulation tissue, 1 (25%) biofilm formation, and 1 (25%) stent migration. Two (50%) patients with stents required IBP for tumor recurrence. The number of IBPs performed because of tumor recurrence was 20 (25.9%) (Figure 3).
Figure 3
Bronchoscopic appearance of granulation tissue and tumoral recurrence (distinguishable from each other only after pathologic examination). A1: Partial obliteration of the left distal part of the Y-shaped silicone stent due to tumor recurrence. A2: Total obliteration of the right distal part of the Y-shaped silicone stent due to granulation tissue formation in the same patient. B1: Granulation tissue seen in the tracheal lumen at the proximal part of the Y-shaped airway stent. B2: Tumor recurrence at the right distal part of the Y-shaped silicone stent in the same patient

Follow-up
Patients were followed up with surveillance bronchoscopies according to our institutional IP unit routines. Flexible bronchoscopies were performed after 2 weeks, and at 1, 3, 6 and 12 months following IBP, and earlier when required.
Among 5 patients referred due to suspected tumor recurrence, 4 patients were found to have recurrence and 1 benign stenosis. Three patients with recurrence had silicone stent placement while 1 patient was referred to the oncology clinic after establishing adequate airway patency with mechanical resection. The patient with benign stenosis remains in clinical, radiological and surveillance bronchoscopy following dilatation.
Among 8 patients (61.5%) who were diagnosed at our IP unit, 4 were referred to oncology and 4 to thoracic surgery clinics. Two of these patients subsequently needed additional IBP because of respiratory distress and 1 was treated with stenting. A total of 6 patients (46.2%) were treated for tumor recurrence.
The mean follow-up duration of patients was 38.9 months (range: 7–112). This duration was 67.3 months (range: 38– 112) for patients treated with stents and 15.5 months (range: 4–66) for the remainder. Survival analysis was not possible because of the low number of cases. Four (30.8%) patients died during follow-up. Their median survival time following IBP was 15.5 months (range: 4–44) months (Table 2).
DISCUSSION
ACC are rare malignancies originating from secretory glands of the central airways (tracheobronchial system). Adequate airway patency was established in the vast majority of patients with ACC treated with IBP in our IB unit, providing clinical relief until oncologic or surgical management. Compared with other pulmonary malignancies, ACC is quite different in terms of its clinical course. It affects younger patients who survive longer compared to other pulmonary malignancies and demonstrates high rates of local invasion and recurrence1.
Previous studies have not found an association between smoking status and ACC or a gender predilection for this tumor. In contrast, our study included disproportionately more non-smoking male patients1,2.
Delays in the diagnosis of ACC are common because of the slow progression of the tumor. Likewise, most of our patients had a long-lasting history of bronchodilator treatment for asthma and COPD. There were seven patients with obstructive airway disease, among whom 5 were inoperable at presentation, which might have been related to delayed diagnosis. Malignant airway obstruction should be considered in patients with obstructive airway disease not responding to bronchodilators and inhaled steroids. When patients with ACC develop new symptoms during follow-up, the possibility of disease recurrence should be considered before attributing the symptoms to comorbidities or side effects of oncologic treatment1,2,7.
Surgical resection is the treatment of choice in ACC. Adjuvant radiotherapy or chemotherapy can be added to the treatment depending on the presence of residual tumor at the resection margin8,9. A multidisciplinary approach to the management of ACC involving IP, oncology and thoracic surgery clinics would be beneficial in terms of patient survival and quality of life10,11. IBPs are a palliative treatment option in patients who are not surgical candidates or in cases of recurrence following surgical resection, oncologic treatment or previous IBPs3,6,11. Indeed, we found that IBP contributes to the palliative treatment of these patients.
ACC most commonly involves the trachea according to the literature. Likewise, we found that the trachea was involved in 76.9% of cases. Wang et al.5 reported an 86.5% rate of mixed type bronchoscopic findings consisting of endoluminal involvement, external compression and mucosal infiltration. In contrast, we found that the most common bronchoscopic finding was endoluminal type, while mixed type was present in 46.1%1,12-14.
ACC are tumors with a slow progression with patients having long expected survival times. Rather than invading neighboring organs, tumors tend to grow longitudinally within the lumen, potentially leading to malignant airway obstruction. Therefore, patients with ACC may require repeated IPBs1. Wang et al.5 reported that the mean number of procedures (RB and FB) per patient with mixed involvement was 14. Lee et al.13 reported a mean of 4.1 procedures per patient in their series of 30 patients with ACC. The median number of repeated IBPs for recurrence following surgery and oncologic therapy and airway obstruction in our study was 7.
Kim et al.11 have reported that the success rate of firstline IBP in establishing airway patency was 92.7%. Our success rate with first-line IBP was 93%.
Applied IBP procedures can differ according to availability of the IP unit and physician experience. Usually, a multimodal treatment consisting of APC, cryo, laser and mechanical methods is applied. Mechanical resection and thermal methods (APC, laser) were the most frequently used treatment modalities in Kim et al.11 study population of 57 patients. Mechanical resection and APC were the most common used treatment modalities in our IP unit.
In the study of Lee et al.13, no serious procedural complications or mortality were reported in 82 procedures. In this study, 8 of 20 patients who were treated with airway stents had late stent-related complications such as granulation, mucostasis, and migration. Most repeated IBPs had been applied to these patients13. In their study Wang H et al.5 stated that since the complication rates of repeated IBPs are quite low compared to surgery, they can be used to achieve local control especially in patients with endoluminal component. In our study, a total of 77 procedures were performed. Two patients suffered early complications. One required twice intensive care treatment, once due to moderate hemorrhage and once due to respiratory acidosis; this patient had undergone 34 of the 77 procedures. The other patient developed pneumothorax and was treated with tube thoracostomy. There was no mortality due to these early complications. Late complications were not directly related to IBP but to stents. Similar to the study of Lee et al.13, complications such as granulation, mucostasis, and migration were observed in 3 of 4 patients who were treated with airway stents. Tumor recurrence was detected in 2 patients with airway stents, which cannot be considered as a complication of IBP. Repeated procedures were mostly performed on patients with airway stents. It has been suggested that drug-eluting stents can be used in malignant central airway obstructions15. This can be considered also in ACC due to the high rates of granulation tissue formation seen with standard airway stents and the tumor’s ability to spread longitudinally under the stent.
It has been reported that IBPs increase the survival in patients with malignant airway obstruction16. A statistically significant relationship was found between stenting and survival among the treatment modalities used in ACC treatment. In our study, survival analysis could not be performed due to the low number of cases. It was observed that the follow-up duration of our patients who were treated with airway stents was longer than the average follow-up duration of patients without airway stents6,11. It is known that bronchial involvement in ACC shortens survival. Indeed, bronchial involvement was present in 3 of 4 cases who died in our study. In addition, survival in ACC decreases inversely with age. Among the 4 patients who died, 3 were the cases with the oldest age and their mean age was higher than the average of the study population11,17,18.
Limitations
Limitations of our study include its retrospective nature about a rare type of malignancy and the low number of patients, which precluded statistical calculations on the contribution of interventional procedures on patient survival. Although patients were observed to have less dyspnea following the procedure, this could not be evaluated objectively because of the absence of dyspnea score records.
CONCLUSIONS
ACC is a rare type of pulmonary malignancy involving the central airways and most commonly the trachea. IBPs carry a low rate of early complications even if required to be performed multiple times. Airway stents are used in the palliation of symptoms of central airway obstruction and should be closely followed up for late complications. There is a need for prospective studies to assess the contribution of IBPs in the success of treatment and patients’ quality of life.

