Dear Editor,
Hypertrophic osteoarthropathy (HOA) as a paraneoplastic disorder is most often associated with pulmonary malignancies1. Bone scintigraphy (BS) is known to be useful for detecting HOA1,2. Here, we present a lung cancer patient who demonstrated findings consistent with HOA on BS and somatostatin receptor scintigraphy (SRS). To the best of our knowledge, this is the first report of HOA visualized by SRS.
A female aged 67 years, smoker (47 pack-years), presented with a 3-month history of generalized arthralgia, painful edema of the limps, and finger clubbing. BS using 99mTc-MDP demonstrated increased linear periosteal uptake in the long bones of the legs (Figure 1A), a characteristic scintigraphic pattern of HOA. A chest X-ray was done (given her history of smoking) and showed a mass in the right posterior hemithorax confirmed by computed tomography (CT) scan (Figure 2C). Further functional imaging with SRS using 99mTc-octreotide revealed that the pulmonary lesion was positive for somatostatin receptors (Figure 2D). Also, it showed mildly increased tracer uptake along the periosteum of both lower extremities (Figure 1B). Ultimately, histopathological examination revealed lung adenocarcinoma.
Figure 1
A. BS images show bilateral, linear uptake of the radiopharmaceutical in the femurs and tibia (arrows), findings compatible with the tram line or double stripe sign, and to a lesser degree uptake in the distal upper extremities, including the terminal phalanges (dotted arrows). B. SRS images reveal mildly increased linear uptake, more pronounced along the distal femoral and tibial metaphyses (arrows).
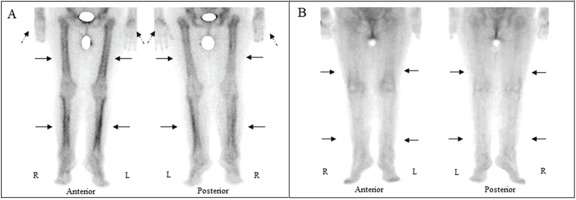
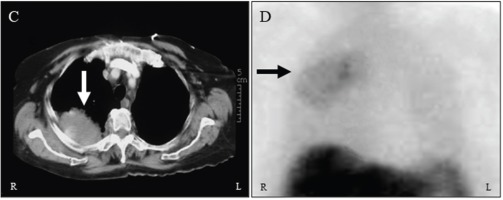
Figure 2
C. CT scan of the chest showing a mass posteriorly in the upper right hemithorax (white arrow). D. Planar SRS anterior image of the chest demonstrating increased tracer activity corresponding to the lesion visualized on the CT scan (black arrow). Note the physiological intense uptake in the liver and spleen.
ΗΟΑ, also named Marie–Bamberger syndrome was first described in the 1890s and is characterized clinically by periostitis of tubular bones, digital clubbing, and arthritic symptoms1. It can be classified as primary (very rare) or secondary (approximately 95% to 97% of cases). Secondary HOA is associated with a wide spectrum of diseases, including a variety of pulmonary disorders, also known as ‘hypertrophic pulmonary osteoarthropathy’ (e.g. primary and metastatic lung cancer, lung abscess, tuberculosis, sarcoidosis, emphysema, bronchiectasis, pulmonary fibrosis, and mesothelioma), cardiovascular disorders (e.g. cyanotic congenital heart disease, infective endocarditis), gastrointestinal disorders (inflammatory bowel disease and hepatic cirrhosis) and various other disorders. Secondary HOA is more frequently related to pulmonary malignancies (in up to 90%), especially lung cancer1. According to published reports, 4% to 32% of lung cancer patients develop HOA3. The clinical manifestations of HOA may precede the diagnosis of the underlying disease. BS is a sensitive imaging modality for evaluating a wide variety of skeletal disorders, including HOA1,2. This modality has higher sensitivity for detecting bone metastases in patients with lung cancer compared to SRS4,5. The exact mechanism of pathogenesis of HOA and clubbing remains unknown. Two models have been proposed: a neurogenic pathway and a humoral pathway. In the neurogenic pathway, diseased organs innervated by the vagus nerve induce a neural reflex leading to vasodilatation and increased blood flow to the extremities6. In the humoral pathway cytokines and growth factors (platelet-derived growth factor, prostaglandin E, and vascular endothelial growth factor) induce connective tissue and periosteal proliferation1.
Our case report highlights the usefulness of BS in detecting HOA and the importance of additional (anatomical and functional) chest imaging in the evaluation of malignancy-related HOA. Additionally, this case report shows that SRS can identify HOA, which is a new addition to the literature regarding the range of potential scintigraphic imaging of this syndrome. Moreover, it lends credence to the therapeutic option of octreotide (a synthetic analogue of somatostatin) for symptomatic treatment of HOA3,7-10.

