INTRODUCTION
Precapillary pulmonary hypertension (PH) remains a rare entity, characterized by elevated pulmonary artery pressures which lead to an increase in right ventricular afterload and consequently to impairment of ventricular interdependence1,2. These hemodynamic alterations not only produce the debilitating symptoms of dyspnea and fatigue, but also result in cognitive impairment and peripheral muscle dysfunction3-5. Therefore, the negative influence of PH on patients’ quality of life (QOL) is an anticipated consequence.
To monitor disease progression, guide therapeutic strategies and evaluate drug efficacy, hemodynamic, echocardiographic, biochemical and exercise testing parameters have been used according to existing guidelines6,7. Patient-reported outcomes such as health-related QOL (HRQOL) are now being established in chronic, medical conditions integrating the patient’s perspective8,9. In this context, HRQOL questionnaires are useful tools that can be applied on an individual basis, providing a more holistic evaluation of patients’ physical and mental health10.
The purpose of this study was to investigate potential factors affecting physical and mental HRQOL in patients with precapillary PH (PH-Groups 1, 3, or 4) by utilizing the Minnesota living with pulmonary hypertension questionnaire (MLHF-PH) and the Short form 36-item health survey (SF-36).
METHODS
Study design, participants and data collection
We conducted a prospective cross-sectional analysis of HRQOL questionnaires in individuals with precapillary PH using the SF-36 and the MLHF-PH. Between January and February 2019, 73 consecutive patients, aged >18 years, with hemodynamically confirmed precapillary PH who were previously classified in PH-Groups (1, 3, or 4) and followed up in two Greek PH-referral centers, completed both questionnaires either on follow-up appointments or by telephone interview, and deemed eligible for this study. All included patients were clinically stable, evaluated in the PH outpatient clinic the last 3 months and received PH-specific therapies based on the European PH Guidelines7. Those with postcapillary PH due to left heart disease and individuals experiencing serious mobility problems, due to previous stroke or surgery, were excluded. Demographic, clinical and hemodynamic variables, six-minute walk distance (6MWD) values and World Health Organization Functional Class (WHO FC) were provided by a physician who was blinded to patients’ responses.
The study was approved by the local ethics committee at both centers and conducted according to the Declaration of Helsinki. Written informed consent was obtained from all patients.
HRQOL questionnaires
We administered the MLHF-PH, after legal permission, a validated modified version of the Minnesota living with heart failure questionnaire11. The MLHF-PH consists of 21 questions about the influence of PH on physical, emotional and social aspects of life, producing scores ranging 0–105 (MLHF-PH Total), with lower scores indicating better quality of life11. Two separate scores can also be calculated, one that is produced by 8 questions and refers to physical health (MLHF-PH Phys) and one that is produced by 5 questions and refers to emotional status (MLHF-PH Emot). Concurrently, we administered the SF-36, a widely used tool for self-assessment of physical and mental health status12,13. It consists of 36 questions yielding scores from 0 (worse) to 100 (best) in eight health-specific domains: physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, and mental health. From them, ‘physical functioning’ and ‘role physical’ are correlated most highly with physical status, while ‘role emotional’ and ‘mental health’ are correlated most highly with mental status12.
Statistical analysis
Continuous variables are presented as mean ± standard deviation or as median (interquartile range) as appropriate, while categorical variables as frequencies (n) and percentages (%). Student’s t-test was used to compare a continuous variable normally distributed between two independent groups, and the Mann-Whitney U-test was used as the non-parametric equivalent test. The Kruskal-Wallis method (with post hoc Dunn’s test) was used to compare a continuous variable between more than two independent groups. Categorical variables were compared with the chi-squared test. Pearson’s correlation coefficient was utilized to analyze the linear correlation between two quantitative and normally distributed variables, and Spearman’s correlation coefficient was the non-parametric equivalent test. Cronbach’s alpha was calculated for both questionnaires as an estimate of their reliability.
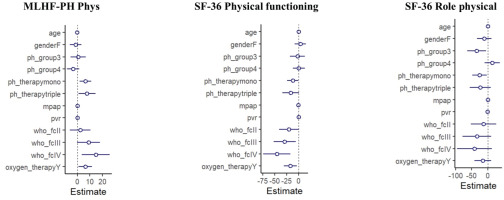
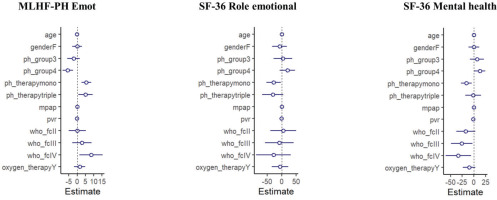
Univariable linear regression analyses were conducted to identify clinical, functional or hemodynamic predictors of physical (MLHF-PH Phys, SF-36 physical functioning and role physical) and mental (MLHF-PH Emot, SF-36 role emotional and mental health) HRQOL domains. A multivariable regression analysis model was then performed for each score, adjusted for the following covariates: age, gender, PH-Group, PH-specific therapies, mean pulmonary artery pressure (mPAP), pulmonary vascular resistance (PVR), WHO FC, and oxygen treatment. Multicollinearity was assessed with the variance inflation factor (<5 suggested absence of multicollinearity). Two-tailed p-values <0.05 were considered significant. All data analyses were performed with the R version 4.3.2 (www.r-project.org).
RESULTS
Patients’ characteristics
SF-36 and MLHF-PH were evaluated in 73 consecutive patients (mean age 60.6 years, 69% female). Demographic, clinical, functional and hemodynamic characteristics of the population are presented in Table 1. In all, 63% of patients were classified as PH Group 1, 18% as Group 3 due to lung disease, and 19% as Group 4. The median duration since PH diagnosis was 3 years. The majority of patients were under PH monotherapy, while 15% received a triple combination. The most common comorbidities were arterial hypertension, diabetes mellitus, and dyslipidemia. Active smoking was reported only in 6% of the total population. Most patients were classified as WHO FC II (52%) and WHO FC III (34%); half of the total population was under continuous oxygen treatment. The 6MWD values were available in 85% of patients and the median 6MWD was 409 m.
Table 1
Demographic, clinical, functional and hemodynamic characteristics of the studied population (N=73)
[i] BMI: body mass index. PH: pulmonary hypertension. WHO FC: World Health Organization functional class. MLHF-PH: Minnesota living with pulmonary hypertension questionnaire. SF-36: Short form 36-item health survey. CO: cardiac output. CI: cardiac index. mPAP: mean pulmonary artery pressure. PCWP: pulmonary capillary wedge pressure. PVR: pulmonary vascular resistance. SVO2: mixed venous blood saturation. WU: Wood units. NT-proBNP: N-terminal-pro brain natriuretic peptide. 6MWD: six-minute walk distance. IQR: interquartile range.
SF-36 and MLHF-PH scores
Analysis of the separate domains of the two questionnaires revealed that PH had a profoundly negative impact on patients’ HRQOL. Specifically, the mean MLHF-PH Total score was almost 50 and the median SF-36 sub-scores were ≤50 in five out of the eight domains (Table 1). ‘General health’ was assessed as moderately impaired by most patients and clinical worsening was anticipated. More than half of patients reported impaired ‘physical functioning’, as they had limited everyday activities and difficulty in working. Their ‘role physical’ was also influenced. ‘Vitality’ was reduced, with fatigue being present in 38% of the population and complete lack of ‘vitality’ in 11%. ‘Emotional health’ varied more, with anxiety feelings in 34.2%, depression in 50%, happiness in 34.2% and calmness in 31.5%.
Factors associated with HRQOL scores
Women, compared to men, presented a trend towards better MLHF-PH Total score (median score 37 vs 53, respectively, p=0.057) and MLHF-PH Phys score (median score 17.5 vs 25, p=0.052); they also had a greater SF-36 ‘physical functioning’ score (median score 45 vs 25, p=0.02). However, their mental status was not significantly different compared to the male sub-population (MLHF-PH Emot, p=0.59; SF-36 role emotional, p=0.71; SF-36 mental health, p=0.27). Age, marital status and level of education were not associated with HRQOL.
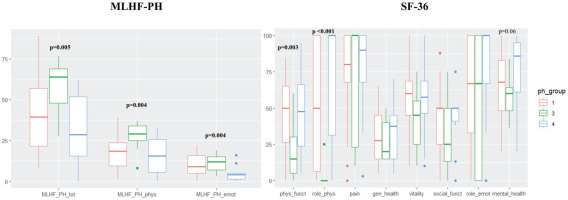
Patients with PH due to lung disease (Group 3) presented significantly worse scores on MLHF-PH compared to the other PH-Groups (Table 2). Furthermore, they had significantly reduced scores in SF-36 ‘physical functioning’ and ‘role physical’ (Table 2). These patients were more frequently under oxygen therapy (p<0.001) and had a more advanced WHO FC (p=0.01). However, differences in hemodynamic parameters between PH-Groups were not evident (Supplementary file Table S1). Graphical presentations of MLHF-PH and SF-36 scores for the different PH-Groups are given in Figure 1. Patients under triple combination PH-therapy had also significantly worse HRQOL scores, both in the physical and mental domains (Supplementary file Table S2).
Table 2
HRQOL in different PH-Groups
| Group 1 Median (IQR) | Group 3 Median (IQR) | Group 4 Median (IQR) | p | |
|---|---|---|---|---|
| MLHF-PH | ||||
| Total | 39.5 (35.5) | 64.0 (21.0) | 28.5 (36.3) | 0.005 |
| Physical component | 18.5 (14.3) | 29.0 (9.0) | 15.5 (20.3) | 0.004 |
| Emotional component | 9.0 (10.8) | 12.0 (8.0) | 4.0 (3.7) | 0.004 |
| SF-36 | ||||
| Physical functioning | 50.0 (38.8) | 15.0 (25.0) | 47.5 (42.4) | 0.003 |
| Role physical | 50.0 (93.7) | 0 | 100 (68.8) | <0.001 |
| Bodily pain | 80.0 (32.0) | 100 (77.0) | 90.0 (32.0) | 0.808 |
| General health | 27.5 (30.0) | 20.0 (25.0) | 37.5 (30.0) | 0.862 |
| Vitality | 60.0 (23.8) | 45 (30.0) | 57.5 (22.6) | 0.208 |
| Social functioning | 50.0 (25.0) | 25.0 (37.0) | 50.0 (9.0) | 0.265 |
| Role emotional | 67.0 (67.0) | 67.0 (100) | 100 (33.0) | 0.426 |
| Mental health | 68.0 (35.0) | 60.0 (16.0) | 86.0 (34.0) | 0.06* |
Figure 1
Box-and-whisker plots demonstrating the sub-scores of the Minnesota living with pulmonary hypertension questionnaire (MLHF-PH) and the Short form 36-item health survey (SF-36) for the different PH-Groups
A significant correlation of all scores of MLHF-PH with mPAP, PVR and mixed venous blood saturation (SVO2) was observed (Table 3). Moreover, increased mPAP and PVR were correlated with deterioration in SF-36 ‘physical functioning’ (mPAP: r= -0.28, p=0.01; PVR: r= -0.24, p=0.04) and in SF-36 ‘general health’ (mPAP: r= -0.24, p=0.04) (Table 3).
Table 3
Correlations† between HRQOL and hemodynamic parameters
† r-correlation coefficients and p-values were produced using Pearson’s or Spearman’s correlation test, as appropriate. Bold values denote statistical significance. HRQOL: health-related quality of life. mPAP: mean pulmonary artery pressure. PVR: pulmonary vascular resistance. SVO2: mixed venous blood saturation. WU: Wood units. MLHF-PH: Minnesota living with pulmonary hypertension questionnaire. SF-36: Short form 36-item health survey.
Oxygen treatment was related to worse HRQOL in terms of physical (MLHF-PH Phys, SF-36 physical functioning, SF-36 role physical; all p<0.001) and emotional (MLHF-PH Emot, SF-36 role emotional, SF-36 mental health; all p<0.001) status. Regarding functional indices, 6MWD and Borg scale presented strong correlations with MLHF-PH scores as well as SF-36 physical domain scores (physical functioning, role physical, general health) and SF-36 ‘mental health’ (Table 4). Patients, categorized in advanced WHO FC, reported poor HRQOL scores.
Table 4
Correlations† between HRQOL, functional and neurohormonal parameters
| 6MWD (m) (N=62) | Borg scale (N=59) | NT-proBNP (pg/mL) (N=40) | ||||
|---|---|---|---|---|---|---|
| MLHF-PH | r-coeff | p | r-coeff | p | r-coeff | p |
| Total | -0.59 | <0.001 | 0.6 | <0.001 | 0.26 | 0.11 |
| Physical component | -0.58 | <0.001 | 0.67 | <0.001 | 0.24 | 0.132 |
| Emotional component | -0.47 | <0.001 | 0.36 | 0.005 | 0.20 | 0.216 |
| SF-36 | ||||||
| Physical functioning | 0.65 | <0.001 | -0.63 | <0.001 | -0.32 | 0.04 |
| Role physical | 0.32 | 0.01 | -0.40 | 0.001 | -0.20 | 0.213 |
| Bodily pain | 0.04 | 0.740 | -0.17 | 0.192 | 0.13 | 0.425 |
| General health | 0.36 | 0.004 | -0.27 | 0.03 | -0.1 | 0.528 |
| Vitality | 0.46 | <0.001 | -0.38 | 0.003 | -0.29 | 0.06* |
| Social functioning | 0.40 | 0.001 | -0.38 | 0.003 | -0.004 | 0.981 |
| Role emotional | 0.09 | 0.483 | 0.02 | 0.897 | -0.04 | 0.804 |
| Mental Health | 0.54 | <0.001 | -0.24 | 0.06* | -0.08 | 0.602 |
Predictors of HRQOL
Univariable regression analyses of physical (MLHF-PH Phys, SF-36 physical functioning, SF-36 role physical) and mental (MLHF-PH Emot, SF-36 role emotional, SF-36 mental health) HRQOL domains are presented in Supplementary file Tables S4 and S5. After multivariable adjustment, the use of PH-specific therapies, advanced WHO FC and use of oxygen treatment, were associated with worse HRQOL physical status (higher MLHF-PH Phys score, lower SF-36 physical functioning score) (Figure 2). Regarding HRQOL mental status, PH-specific therapies and advanced WHO FC but no oxygen treatment, were related to worse scores (higher MLHF-PH Emot score, lower SF-36 role emotional and mental health scores) (Figure 3). PH-Group 3 was independently associated with SF-36 ‘role physical’ (β= -34.3; 95% CI: -63.6 – -5.1, p=0.02), whereas PH-Group 4 was independently associated with MLHF-PH Emot (β= -5.6; 95% CI: -8.7 – -2.6, p<0.001), after adjustment for all other covariates in the model.
DISCUSSION
This prospective cross-sectional study aimed to investigate HRQOL in patients with precapillary PH, and explore the relation of HRQOL questionnaires with clinical, hemodynamic, and functional parameters. The MLHF-PH and SF-36 instruments were used, since they have been previously established in the assessment of QOL in PH11,14. Our analysis demonstrated that QOL was impaired in PH patients. Participants had a score near or lower than 50 (0=worse, 100=best) in several domains of the SF-36, emphasizing the disease burden on both physical and mental status of this peculiar population15.
Patients with PH due to lung disease (PH-Group 3) reported worse QOL, indicated by the significantly worse scores in MLHF-PH compared to the other groups. Physical domains of the SF-36 also presented significant impairment. We found that this group of patients was more frequently treated with oxygen therapy and had a more affected functional status, as reflected by the advanced WHO FC, but without hemodynamic differences compared to PH-Groups 1 and 4. After adjustment, PH-Group 3 emerged as an independent predictor of one of the physical domains in SF-36 (SF-36 role physical). These findings are in line with the study by Brewis et al.16 which compared 188 patients with severe PH due to lung disease with 74 patients with idiopathic PH (PH-Group 1), and showed that patients with pulmonary disorders were more hypoxemic, had worse FC, and achieved lower 6MWD16. Our study possibly reflects that a poorer QOL might be anticipated in this population.
In our study, there was also a strong association between oxygen treatment and worse physical and mental aspects of both questionnaires. After adjustment, oxygen use emerged as an independent predictor of worse physical scores (higher MLHF-PH Phys score, lower SF-36 physical functioning score) but not for mental scores. Previous studies have also indicated oxygen to be related to reduced HRQOL in PH patients17,18. These associations could be attributed to embarrassment feelings in public, along with reduced mobility and carrying issues that oxygen users tend to face19,20. Therefore, they may confine themselves indoors, something that inevitably leads to reduced QOL.
Another noteworthy finding was that HRQOL instruments, used in the current study, were also associated with hemodynamic indices (mPAP, PVR, SVO2). Positive correlations of MLHF-PH scores with mPAP and PVR [higher hemodynamic values – higher (worse) score] and negative correlations with physical domains of SF-36 [higher hemodynamic values – lower (worse) score] emphasize the relation of QOL with PH severity. Our group had previously21 demonstrated the significant correlation of hemodynamics in precapillary PH with emPHasis-10, which is another well-developed and easy to use HRQOL measure in PH22. Functional impairment as a consequence of the disease tended to have an evident impact on patients’ HRQOL, shown by the correlations of WHO FC and 6MWD with the majority of questionnaire scores. WHO FC, a known determinant of HRQOL17,21, was also a multivariable independent predictor in the current study. Furthermore, the strong correlation of MLHF-PH Emot score with hemodynamics in the studied population, highlights the potentially emotional impact of disease severity apart from functional limitations.
Triple combination PH-therapy, which includes the use of prostanoids, as add-on treatment to previously concomitant administration of endothelin receptor antagonists and phosphodiesterase type 5 inhibitors, was strongly associated with diminished state of health. The complexity of administration of these medications (mainly by intravenous or subcutaneous infusion) along with the frequently experienced adverse effects, may be responsible for the impact on patients’ QOL. In a recent British study, researchers explored the differences in QOL between various administration modes of prostanoids and found that intravenous administration was related to the most affected health state (assessed with the EQ-5D-5L instrument)23.
Limitations
The current study has several limitations, since it was an observational design study, conducted on a short-term basis. Therefore, only associations between HRQOL scores and independent variables can be established. Another important limitation is the small number of included patients, which is evident in between-group analyses as well. However, the limited number of participants is probably related to the limited population of northern Greece. Moreover, it is worth mentioning that there was a significant proportion of PH-Group 3 and operable PH-Group 4 patients in outpatient clinics, who were not offered medical treatment and thus were excluded from the study. Regarding hemodynamic variables, they were included from a right heart catheterization having been performed within 12 months before or after the questionnaire completion. The mean time was calculated at 7 months. Finally, HRQOL assessment was not available at the time of PH diagnosis, before the initiation of PH-specific therapies so that comparisons between and after treatment initiation could be conducted.
CONCLUSIONS
Patients with precapillary PH had impaired QOL. Those with PH due to lung disease reported the worst scores in HRQOL instruments (in both physical and mental domains). Several clinical, functional and hemodynamic factors were associated with reduced QOL. Oxygen use and WHO functional class were independent predictors of patients’ physical and mental HRQOL status.