INTRODUCTION
Cutaneous metastases from lung cancer are rare, occurring in 0.22–12% of cases1. Their presence has generally been considered a sign of an already disseminated, poor-prognosis and non-surgical disease2. Nowadays, due to overall improved survival of cancer patients, its incidence is increasing3,4 and it can be the first clinical sign of a new or recurrent malignancy, so the clinician should be alert to recognize it4,5.
Previous data suggest that cancer of the upper lobes is the most likely to metastasize to the skin4,6. Large cell carcinoma and adenocarcinoma are the most common histologic types, while small cell carcinoma is a less frequent cause4,5,7. The malignant lesions tend to appear near the primary tumor, typically at a location on the thorax, followed by the abdomen, head, and neck1,4, and its classical appearance is as a solitary dermal nodule3,5. It is more frequently found in men, being the second most common type of tumor, after melanoma, to metastasize to skin; whereas breast cancer (70%) accounts for the overwhelming majority of cases in women4,5.
Clinical rationale for the study
Limited research has been published on cutaneous metastases in recent years. To fill this gap this study analyzes 25 years of data of patients with lung cancer and cutaneous metastases and their survival8.
METHODS
Study design and subjects
The main objective of this study is to evaluate the survival of patients with cutaneous metastases caused by lung cancer, as confirmed by skin biopsy.
As secondary objectives, the prevalence of cutaneous metastases in the lung cancer population, the population characteristics, based on age, gender, smoking history, histology of primary tumor, staging, location, type and number of skin lesions, extracutaneous metastases, and identification of risk factors, were analyzed.
The patients included were adults (aged ≥18 years), with lung cancer and a skin lesion confirmed histologically to be a cutaneous metastasis. Patients with suspicious cutaneous lesions without a skin biopsy, were excluded.
Methods
A retrospective study was conducted with patients diagnosed with lung cancer and cutaneous metastases, from January 1995 to December 2020, who either attended the pulmonology outpatient clinic and day hospital or who were in the pulmonology ward, in the Local Health Unit of Guarda.
Data regarding demographic characteristics were collected from clinical records, including smoking history; location and histology of the primary tumor; staging, according to the International Association for the Study of Lung Cancer (IASLC) 8th edition lung cancer staging; number, location and type of skin lesion; histology of skin biopsy; time of diagnosis of lung cancer and cutaneous metastases; other distant metastases; treatment of the primary tumor and history of the disease.
Statistical analysis
Statistical analysis was performed using IBM SPSS v25®. For descriptive analysis, qualitative variables were expressed as absolute numbers and percentages; quantitative continuous variables were expressed as mean and standard deviation or median and interquartile range. A Cox regression model was used to investigate the hazard risk related to demographic characteristics, smoking history, and histology. Survival analysis, specifically overall and after detection of cutaneous metastases, was also performed, with the Kaplan-Meier method and the log-rank test, considering a level of significance of 5%.
RESULTS
From a total of 1172 cases of lung cancer, a cutaneous metastasis was diagnosed by skin biopsy in 11 cases or 0.94% of our population. There were 7 men (63.6%) and 4 women with a median age of 78 years, ranging from 50 to 88 years, and 63.6% with a past or active smoking history. In 6 patients (54.5%), this finding occurred simultaneously with primary lung cancer. For the 5 cases with known pre-existing lung cancer, the interval between first diagnosis and skin biopsy was 7.80 months (range: 0–26). Table 1 summarizes patient features and clinical data.
Table 1
Characteristics of patients with lung cancer and cutaneous metastases
| Sex | Age | Smoking | Previous known LC | Primary lung cancer | Skin lesion | Extracutaneous metastasis | Treatment* | Survival post SB (days) | OS (months) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Histology | Location | Initial staging | Number | Location | Type | ||||||||
| M | 60 | NS | Yes | Adenocarcinoma | RLL | T3N1M0 | 1 | Chest | Plaque | - | Surgery, chemo and radiotherapy | 27 | 27 |
| M | 68 | S | No | Epidermoid | LUL | T4N3M1b | 1 | Perineum | Nodule | Bone | Chemotherapy | 144 | 11 |
| F | 87 | - | Yes | Adenocarcinoma | ML | T2bN3M1a | 1 | Chest | Tumor | Bone | BSC | 26 | 2 |
| F | 78 | NS | Yes | Adenocarcinoma | LUL | T2aN2M0 | 2 | Scalp | Nodule | Bone | Surgery, chemotherapy | 126 | 17 |
| M | 79 | S | No | Adenocarcinoma | LLL | T4NxM1c | 2 | Chest, Gluteal | Nodule | Adrenal | Chemotherapy | 105 | 3 |
| M | 79 | FS | Yes | Adenocarcinoma | RUL | T4N2M1a | 3 | Cervical, Face, Dorsal | Nodule | - | Chemotherapy | 12 | 1 |
| F | 63 | NS | No | Adenocarcinoma | LLL | T3N2M1a | 1 | Dorsal | Ulcer | Bone | Chemotherapy | 82 | 2 |
| M | 56 | S | No | Adenocarcinoma | RUL | T2aN2M1c | 1 | Abdominal | Nodule | Liver, bone | BSC | 19 | 0 |
| M | 80 | FS | No | Epidermoid | LLL | T4N3M1c | 1 | Abdominal | Nodule | Liver | BSC | 12 | 0 |
| M | 88 | FS | No | Neuroendocrine | RUL | T4N1M1c | 1 | Dorsal | Nodule | Adrenal | BSC | 35 | 1 |
| F | 50 | FS | Yes | Neuroendocrine + Adenocarcinoma | RLL | T4N2M1b | 2 | Abdominal, Chest | Nodule | - | Chemotherapy, Immunotherapy | 554 | 19 |
The main location of the primary tumor was the right upper lobe and the left lower lobe, with 3 cases each. There was an overall predominance of the tumors from the right lung (6 cases). The distribution by histological type of the primary tumor was as follows: 7 cases of adenocarcinoma (63.6%), 2 cases of squamous cell carcinoma (18.2%), 1 large cell neuroendocrine carcinoma, and 1 small cell neuroendocrine combined with adenocarcinoma. In 7 patients, cutaneous metastases developed as a single lesion, the other 4 patients had between two and three skin lesions. The main presentation was a nodule (72.7%), located in the anterior chest wall (4 cases), followed by upper abdominal wall (3 cases) and torso (2 cases).
Of the 8 patients who underwent lung biopsy, all the skin lesions had histological concordance with lung primary tumor. Considering the clinical stage by the time of the diagnosis of lung cancer, 5 were in stage IV-A, 4 in IV-B, and 2 in III-A. Eight patients (72.7%) had extracutaneous metastases, predominantly in bone in 5 of the cases.
In the majority of the cases who were suitable to initiate treatment, chemotherapy was administered, either alone or in combination with surgery and/or radiotherapy. In four cases, they were given the best supportive care. Only one case, our last patient, has underwent both chemotherapy and immunotherapy.
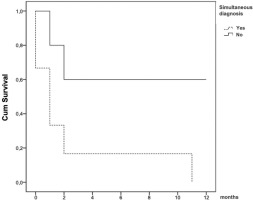
Due to the small number of cases, statistical evaluation for prognostic factors were not significant in this population. In this population, the median overall survival was 2 months (range: 0–27), while survival from the diagnosis of cutaneous metastases was 1 month (range: 0–18). Survival analysis revealed that the diagnosis of cutaneous metastases at the same time as lung cancer shortens survival with statistical significance (2.50 vs 13.20 months; p=0.032) (Figure 1). The presence of extracutaneous metastases (4.25 v. 15.67 months; p=0.157) and smoking history (4.86 vs 15.00 months; p=0.167), as the number of skin lesions, one vs more than one (mean 6.00 vs 9.75 months; p=0.220), tend to decrease survival time; nevertheless, without statistical significance.
DISCUSSION
This 25-year retrospective study has demonstrated the rarity of the presence of cutaneous metastases in lung cancer (0.94%), which is in accordance with the literature.
The main histological type found was adenocarcinoma, which is also the most prevalent subtype of lung cancer worldwide9-11, followed by squamous cell carcinoma. Concerning the location of primary lung cancer, no predominance in the upper lobes without considering the middle lobe ‘as part of’ the right upper part of the lung was found; however, there was a predominance of the right-side12.
Cutaneous metastases can occur in any site on the skin surface. These data emphasized that almost three quarters (72.7%) had skin lesions in the anterior and posterior chest wall, face and scalp, near the primary tumor, representing <30% of body surface area4,12. The only exception was the case that had a single nodule in the perinium, a very rare location1,13,14.
The survival was more affected by the number of metastasized organs, rather than by the number of skin lesions. The presence of extracutaneous metastases shortens the survival time by almost a year, although not statistically significant. The number of skin lesions, one vs more than one, decreases the survival time to a much less extent than was expected12, with a difference of 4 months shorter for those with more than one skin lesion, requiring the clinician to be more alert to search for these on a daily basis.
This research reinforces the importance of smoking habits in the evolution and progression of lung cancer. A past or active smoking history at the time of diagnosis also decreases mean survival time by almost a year15. Worldwide and national policies should never stop emphasizing, to children, teenagers, and adults, the importance of non-smoking habits to improve health and limit secondhand smoke exposure16.
The only finding with statistical significance was the synchronous diagnosis of lung cancer with cutaneous metastases. When lung cancer is diagnosed simultaneously with the cutaneous metastases, the prognosis is terrible, with a median survival time of 1 month. An ‘outlier’ of this inference is the last diagnosed patient, which has a combined histological lung cancer, small cell neuroendocrine carcinoma and adenocarcinoma, with mutations by new generation sequencing (NGS) and PD-L1 both negative, diagnosed simultaneously with a skin biopsy histologically in accordance with the lung biopsy. This patient was the first of the sample who underwent chemotherapy (with platin and etoposide) and immunotherapy (with atezolizumab). At present, her overall survival is close to 2 years, which opens the discussion for further investigation on whether immune checkpoint inhibitors can improve the survival of these patients, since it was first proved beneficial in metastatic melanoma17.
Limitations
In a retrospective study extending to such a long time period, there are certain limitations on obtaining data from the years when medical records were not computerized. One of the difficulties the authors had was the inaccessibility of chest computed tomography images required to re-stage, especially the tumor size (T) of those patients, according to the IASLC 8th edition lung cancer staging, since some reports lack some current relevant information that, in the previous century, was not taken into consideration.
Also, the small number of cases of lung cancer patients with cutaneous metastases, which is in accordance with published data, makes statistical inferences more difficult to reach, as seen in other studies. Since no patient had a treatment directed to their cutaneous metastasis, more studies and a bigger sample would be needed to clarify if this would have any impact on overall survival. Another bias of this study is that not all lung cancer patients with suspicious skin lesions, underwent a skin biopsy, especially those with end-stage disease.
Clinical implications and future directions
This 25-year experience emphasizes the importance of clinicians being alert to the possibility of skin lesions, either during the diagnostic approach or the follow-up of lung cancer patients, in order to identify as early as possible these patients with poor prognosis and give them the best therapeutic option. Finally, our last patient opens a window of possible future investigation into the treatment of these patients with immunotherapy, not just for lung cancer itself, but for the presence of cutaneous metastases.