INTRODUCTION
Mediastinal hematoma is a significant and potentially fatal iatrogenic complication, well-described by thoracic surgeons, as a result of dissection of major vessels. Spontaneous non-traumatic hematomas have also been described and attributed to anticoagulant medication1. Severe consequences of mediastinal hematoma include cardiac tamponade, compression of the esophagus, abscess formation, and shock.
Conventional and endobronchial ultrasound guided (EBUS) transbronchial needle aspiration (TBNA) are well-established methods for sampling mediastinal enlargements. EBUS-TBNA has also been used for transvascular approach for sampling lesions located behind the aorta or the pulmonary artery with acceptable safety profile.
Here, we report on a case of hemomediastinum developed several days following an uneventful EBUS-TBNA procedure in a patient reassuming his anticoagulant treatment after discharge from the hospital.
CASE PRESENTATION
A 74-year-old man, with a smoking history of 50 pack-years, presented in the Interventional Pulmonology Unit for mediastinal lymph node enlargement, complaining of chronic cough since 2 months and weight loss (>8 kg) in the last 6 months. His medical history was remarkable for aortic valve replacement with metallic graft under acenocumarol, chronic obstructive pulmonary disease under tiotropium inhalations, hyperlipidemia, and hepatitis B carriage. The physical examination and blood analysis were normal except for prolonged INR (3.82) presumably due to the vitamin K inhibitors.
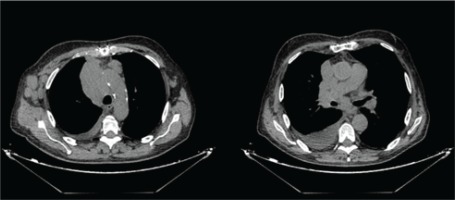
The patient had a chest CT (computed tomography) done without iv (intravenous) contrast 2 days before his admission (Figure 1). The CT scan of the thorax showed an enlarged lymph node block (8.8 × 5.2 cm) in the right paratracheal region (4R), enlarged lymph nodes in the subcarinal level (7) and right hilum, as well as a moderate pleural effusion in the right hemithorax. Ideally, iv contrast material should have been administered to assess the mediastinum, but the patient had just performed this CT and a repeat with iv contrast was not deemed necessary. Furthermore, on CT, an extrathoracic, not clinically palpable lymph node in the lower cervix was also noticed. No solid mass was observed in the lung parenchyma except for a 5.5 mm solid nodule in the left lower lobe. Brain and abdomen CTs showed no distant metastasis. The pulmonary function test revealed a non-reversible moderate obstruction pattern (FEV1pred: 51%, FEV1/FVC: 0.59).
Minimally invasive procedures such as bronchoscopy are preferred to mediastinoscopy, given that the target is reachable being adjacent to the airways. Direct visualization of the puncture site is also preferable. Thus, indication for bronchoscopy was clear and the patient was scheduled for EBUS-TBNA (endobronchial ultrasound transbronchial needle aspiration). The differential diagnosis of the enlarged lymph nodes included lymphoproliferative or granulomatous diseases (tuberculosis or sarcoidosis) and lung cancer.
The vitamin K inhibitors were discontinued for 4 days and replaced with low molecular weight heparin (tinzaparin once daily in therapeutic dosage). After the prothrombin time was normalized (INR: 1.2) pleural drainage in the right side was performed with inconclusive cytology of a lymphocytic exudate (lymphocytes: 86%) with low ADA values (6.86 IU/dL).
EBUS-TBNA was performed with an Olympus Optical Co. Ltd. Tokyo, Japan, BF type UC 180F ultrasound bronchoscope. The procedure was performed under conscious sedation (midazolam and fentanyl) and local instillation of lidocaine under continuous monitoring of oxygen saturation, blood pressure and ECG.
No endobronchial lesion was identified, and EBUS revealed an inhomogeneous, hypoechoic lymph node enlargement with observable margins in the right paratracheal area (LN station 4R) as well as a similar one in the subcarinal area (LN station 7) (Figure 2).
A standard Olympus 21 G cytology needle was used for the EBUS-TBNA, and the samples were assessed for adequacy with rapid on-site evaluation (ROSE). The 4R LN station was sampled first three times with 8–10 passes of the needle, followed by the 7 LN station which was sampled three times as well with similar needle passes. ROSE by the pulmonary endoscopists was reported with adequate lymphocytic representation and several suspicious cells. The procedure was completed uneventfully, the patient returned to his ward and was discharged the following day with the advice to reassume his vitamin K inhibitor treatment. Amoxicillin/clavulanate (500/125 mg × 3 per day) was also prescribed for 10 days.
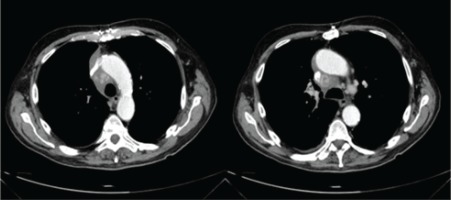
Three weeks later the patient presented to the Emergency Department due to low grade fever for the past two weeks, persistent cough and mild exertional dyspnea. His laboratory results were notable for a supratherapeutic INR of 5.36 and high CRP (15.5 mg/dL). A chest CT with iv contrast was performed (Figure 3) and revealed a right paratracheal fluid collection radiologically consistent with hematoma and with disintegration of the paratracheal lymph node of the 4R station. The paratracheal hematoma (+45 Hounsfield units) was correlated to the supratherapeutic INR and the recent bronchoscopy with EBUS-TBNA. It could also be hypothesized that the antibiotic regimen altered the metabolism of the vitamin K antagonist leading to supratherapeutic levels of anticoagulation.
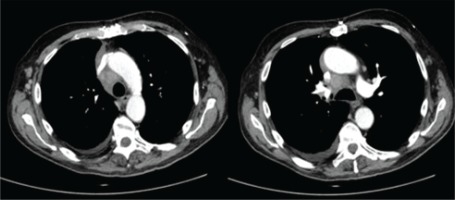
Thoracic surgeons recommended watchful waiting and withholding anticoagulation until return to therapeutic values. Antibiotic treatment was upgraded to piperacillin-tazobactam and linezolid. INR was normalized (1.06) 3 days later. The patient recovered as symptoms and fever subsided on day 3 of hospitalization. Repeat imaging 12 days later showed improvement of the mediastinal hematoma (Figure 4) after which anticoagulation was resumed. The patient was then discharged safe.
The histology of the EBUS-TBNA specimen was found to be inconclusive due to necrosis, and the patient was scheduled for surgical biopsy aiming diagnosis of the lymphadenopathy. The final diagnosis was follicular lymphoma (non-Hodgkin).
DISCUSSION
Mediastinal bleeding and development of hematoma (hemomediastinum) can rarely occur after TBNA, most often due to the accidental puncture of a great vessel2-4. Although scarce case reports exist in the literature, this has not been confirmed in large safety assessment studies of TBNA5. Even more, transvascular approach is deemed safe6,7. The intentional puncture of a left hilar mass through the pulmonary artery has been reported in 10 cases without producing any complication, arguing for the safety of the technique with low-pressure vessels. On the other hand, in a series of 14 cases of trans-aortic puncture for para-aortic lymph node or masses with 22-gauge needles led by endoscopic ultrasonography, 2 cases of para-aortic hematomas occurred8, arguing probably also for the safety of the technique with high-pressure vessels.
Iatrogenic post TBNA mediastinal hematoma (non transvascular) has both been reported with the thin cytology 21G needle2 or with the larger histology 19G needle4. It has been equally reported after conventional TBNA2-4 or most recently with EBUS guided TBNA9-11, a directly observed modality with which it was formerly thought that this complication would be avoided. Although most often the mediastinal bleeding and the acute retrosternal thoracic pain it produces are self-limited and spontaneously resolving, there have been cases with life threatening complications such as hemopericardium leading to tamponade12. Further complication of hematoma with infection is possible, and life threatening mediastinitis or mediastinal abscess formation can occur after EBUS-TBNA13-15.
All seven published case reports of post TBNA mediastinal hematomas refer to the most commonly sampled LN stations (4R, 4L, 7) and to patients with no bleeding diathesis or current anticoagulation treatment, except one regarding a patient who reassumed his warfarin treatment (in increased dosage) after an uneventful procedure developing hematoma 5 days post discharge from the hospital11 (Table 1). In most of the cases there was spontaneous resolution of the hematoma/hemomediastinum.
Table 1
Case reports of mediastinal bleeding complications post TBNA
| Authors Year | Age (years) Gender | Technique Type of needle | Lymph node station | Final diagnosis | Complication | Symptoms/Findings | Anticoagulation | Treatment |
|---|---|---|---|---|---|---|---|---|
| Kucera et al.2 1985 | 49 Male | Conventional TBNA Not specified | A-P window, 7, 4R | Unknown | Hemomediastinum after accidental puncture of the aorta | Chest pain | No | Spontaneous resolution |
| Lazzari Agli et al.3 2002 | 57 Male | Conventional TBNA 22G cytology needle | A-P window | Non-small cell lung cancer | Mediastinal periaortic hematoma after accidental puncture of the aorta | Chest pain, chills, sweat | No | Spontaneous resolution |
| Talebian et al.4 2004 | 65 Female | Conventional TBNA 22G cytology needle | 4R | Sarcoidosis | Hemomediastinum after inadvertent penetration of the anterior wall of the trachea | Retrosternal chest pain, soft tissue enlargement over left supraclavicular region | No | Spontaneous resolution |
| Gross et al.12 2011 | 65 Male | Conventional TBNA 21G needle | 4R | Adenocarcinoma | Cardiac tamponade after transpericardial puncture of a major vessel (a pericardial fold was misinterpreted as a lymph node) | Intense back pain and pericardial fluid on cardiac ultrasound | No | Pericardiocentesis and pericardial fenestration |
| Botana-Rial et al.9 2012 | 62 Male | EBUS TBNA 21G cytology needle | 4L | Non-small cell lung cancer | Pulmonary artery intramural hematoma after accidental puncture of the pulmonary artery | Sonographic crescent image at the top of pulmonary artery | No | Spontaneous resolution |
| Torky et al.10 2017 | 70 Male | EBUS TBNA 22G cytology needle | 4L, 10L | Non-small cell lung cancer | Mediastinal hematoma after accidental puncture of abnormally located bronchial artery | Disturbance of the sonographic appearance of the mediastinum during sampling | No | Spontaneous resolution |
| Patel et al.11 2020 | 66 Female | EBUS TBNA 22G cytology needle | 7, 10L | Anaplastic lymphoma | Subcarinal mediastinal hematoma | Dysphagia due to esophageal compression by the hematoma | Warfarin for metallic aortic valve bridged with enoxaparin | Holding anticoagulation for 24 hours |
Similarly, the patient reported here, underwent bronchoscopy having discontinued his anticoagulation treatment and reassumed his treatment the following day which unexpectedly a few days later led to supratherapeutic values producing the bleeding and the formation of hematoma. Interestingly, our patient after bronchoscopy was initiated with amoxycillin/clavulanate together with his usual dosage of acenocumarol. Coumarin anticoagulants have well known drug-drug interactions and their concomitant use especially with amoxycillin (alone or with clavulanate) is associated with major bleeding16. This case raises the suspicion that late onset post TBNA hematomas could occur in the setting of anticoagulation treatment post bronchoscopy.
To the best of our knowledge, this is only the second case reported with late onset mediastinal hematoma post EBUS-TBNA and the first to be attributed to combined amoxycillin treatment and coumarin anticoagulants.
CONCLUSION
Although rare, hemomediastinum is a potential complication of EBUS-TBNA of which pulmonologists should be aware. To our knowledge, there have been only few case reports of mediastinal bleeding following transbronchial or transesophageal (EBUS/EUS) puncture and most of them were not related with coagulation abnormalities. Late onset hematomas can also occur in the setting of anticoagulation treatment post bronchoscopy and close monitoring of INR is warranted to avoid severe or even life-threatening complications.